Get the App
For Doctors
Login/Sign-up
Last Updated: Aug 29, 2019
BookMark
Report
Dr. Govind VermaGastroenterologist • 31 Years Exp.DM - Gastroenterology, MD - General Medicine, MBBS
Gastroesophageal reflux disease, or gerd, is a digestive disorder that affects the lower esophageal sphincter (les), the ring of muscle between the esophagus and stomach. Many people, including pregnant women, suffer from heartburn or acid indigestion caused by gerd. Doctors believe that some people suffer from gerd due to a condition called hiatal hernia. In most cases, heartburn can be relieved through diet and lifestyle changes; however, some people may require medication or surgery.
What is gastroesophageal reflux?
Gastroesophageal refers to the stomach and esophagus. Reflux means to flow back or return. Therefore, gastroesophageal reflux is the return of the stomach's contents back up into the esophagus.
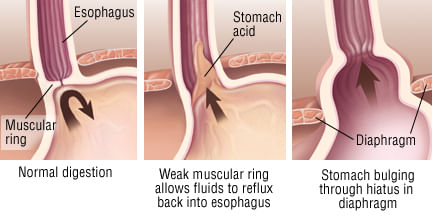
In normal digestion, the lower esophageal sphincter (les) opens to allow food to pass into the stomach and closes to prevent food and acidic stomach juices from flowing back into the esophagus.
Gastroesophageal reflux occurs when the les is weak or relaxes inappropriately, allowing the stomach's contents to flow up into the esophagus.
The severity of gerd depends on les dysfunction as well as the type and amount of fluid brought up from the stomach and the neutralizing effect of saliva.
What is the role of hiatial hernia in gerd?
Some doctors believe a hiatal hernia may weaken the les and increase the risk for gastroesophageal reflux. Hiatal hernia occurs when the upper part of the stomach moves up into the chest through a small opening. Many people with a hiatal hernia will not have problems with heartburn or reflux. But having a hiatal hernia may allow stomach contents to reflux more easily into the esophagus.
Coughing, vomiting, straining, or sudden physical exertion can cause increased pressure in the abdomen resulting in hiatal hernia. Obesity and pregnancy also contribute to this condition. Many otherwise healthy people age 50 and over have a small hiatal hernia. Although considered a condition of middle age, hiatal hernias affect people of all ages.
Hiatal hernias usually do not require treatment. However, treatment may be necessary if the hernia is in danger of becoming strangulated (twisted in a way that cuts off blood supply, called a paraesophageal hernia) or is complicated by severe gerd or esophagitis (inflammation of the esophagus). The doctor may perform surgery to reduce the size of the hernia or to prevent strangulation.
What other factors contribute to gerd?
Dietary and lifestyle choices may contribute to gerd. Certain foods and beverages, including chocolate, peppermint, fried or fatty foods, coffee, or alcoholic beverages, may trigger reflux and heartburn. Studies show that cigarette smoking relaxes the les. Obesity and pregnancy can also play a role in gerd symptoms.
What are the symptoms of heartburn?
Heartburn, also called acid indigestion, is the most common symptom of gerd and usually feels like a burning chest pain beginning behind the breastbone and moving upward to the neck and throat. Many people say it feels like food is coming back into the mouth leaving an acid or bitter taste.
The burning, pressure, or pain of heartburn can last as long as 2 hours and is often worse after eating. Lying down or bending over can also result in heartburn. Many people obtain relief by standing upright or by taking an antacid that clears acid out of the esophagus.
Heartburn pain can be mistaken for the pain associated with heart disease or a heart attack, but there are differences. Exercise may aggravate pain resulting from heart disease, and rest may relieve the pain. Heartburn pain is less likely to be associated with physical activity.
How common is heartburn and gerd?
More than 60 million adults experience heartburn at least once a month, and more than 15 million adults suffer daily from heartburn. Many pregnant women experience daily heartburn. Recent studies show that gerd in infants and children is more common than previously recognized and may produce recurrent vomiting, coughing, and other respiratory problems.
What is the treatment for gerd?
We recommend lifestyle and dietary changes for most people needing treatment for gerd. Treatment aims at decreasing the amount of reflux or reducing damage to the lining of the esophagus from refluxed materials.
Avoiding foods and beverages that can weaken the les is often recommended. These foods include chocolate, peppermint, fatty foods, coffee, and alcoholic beverages. Foods and beverages that can irritate a damaged esophageal lining, such as citrus fruits and juices, tomato products, and pepper, should also be avoided if they cause symptoms.
Decreasing the size of portions at mealtime may also help control symptoms. Eating meals at least 2 to 3 hours before bedtime may lessen reflux by allowing the acid in the stomach to decrease and the stomach to empty partially. In addition, being overweight often worsens symptoms. Many overweight people find relief when they lose weight.
Cigarette smoking weakens the les. Stopping smoking is important to reduce gerd symptoms.
Elevating the head of the bed on 6-inch blocks or sleeping on a specially designed wedge reduces heartburn by allowing gravity to minimize reflux of stomach contents into the esophagus. Do not use pillows to prop yourself up; that only increases pressure on the stomach.
Along with lifestyle and diet changes, doctor may recommend over-the-counter or prescription treatments.
Antacids can help neutralize acid in the esophagus and stomach and stop heartburn. Many people find that nonprescription antacids provide temporary or partial relief. An antacid combined with a foaming agent helps some people. These compounds are believed to form a foam barrier on top of the stomach that prevents acid reflux from occurring.
Long-term use of antacids, however, can result in side effects, including diarrhea, altered calciummetabolism (a change in the way the body breaks down and uses calcium), and buildup of magnesium in the body. Too much magnesium can be serious for patients with kidney disease. If antacids are needed for more than 2 weeks, a doctor should be consulted.
For chronic reflux and heartburn, the doctor may recommend medications to
Reduce acid in the stomach. These medicines include h2 blockers, which inhibit acid secretion in the stomach.
What if heartburn or gerd symptoms persist?
People with severe, chronic esophageal reflux or with symptoms not relieved by the treatments described above may need more complete diagnostic evaluation. Doctors use a variety of tests and procedures to examine a patient with chronic heartburn.
An upper gi series may be performed during the early phase of testing. This test is a special x-ray that shows the esophagus, stomach, and duodenum (the upper part of the small intestine). While an upper gi series provides limited information about possible reflux, it is used to help rule out other diagnoses, such as peptic ulcers.
Endoscopy is an important procedure for individuals with chronic gerd. By placing a small lighted tube with a tiny video camera on the end (endoscope) into the esophagus, the doctor may see inflammation or irritation of the tissue lining the esophagus (esophagitis). If the findings of the endoscopy are abnormal or questionable, biopsy (removing a small sample of tissue) from the lining of the esophagus may be helpful.
Esophageal manometric and impedance studies -- pressure measurements of the esophagus -- occasionally help identify low pressure in the les or abnormalities in esophageal muscle contraction.
For patients in whom diagnosis is difficult, doctors may measure the acid levels inside the esophagus through ph testing. Testing ph monitors the acidity level of the esophagus and symptoms during meals, activity, and sleep. Newer techniques of long-term ph monitoring are improving diagnostic capability in this area.
Does gerd require surgery?
A small number of people with gerd may need surgery because of severe reflux and poor response to medical treatment. However, surgery should not be considered until all other measures have been tried. Fundoplication is a surgical procedure that increases pressure in the lower esophagus. Endoscopic procedures that involve making the les function better or using electrodes to promote scarring of the les are newer options in treatment.
What are the complications of long-term gerd?
Sometimes gerd results in serious complications. Esophagitis can occur as a result of too much stomach acid in the esophagus. Esophagitis may cause esophageal bleeding or ulcers. In addition, a narrowing or stricture of the esophagus may occur from chronic scarring. Some people develop a condition known as barrett's esophagus. This condition can increase the risk of esophageal cancer.
Although gerd can limit daily activities and productivity, it is rarely life-threatening. With an understanding of the causes and proper treatment, most people will find relief.
What is gastroesophageal reflux?
Gastroesophageal refers to the stomach and esophagus. Reflux means to flow back or return. Therefore, gastroesophageal reflux is the return of the stomach's contents back up into the esophagus.
In normal digestion, the lower esophageal sphincter (les) opens to allow food to pass into the stomach and closes to prevent food and acidic stomach juices from flowing back into the esophagus.
Gastroesophageal reflux occurs when the les is weak or relaxes inappropriately, allowing the stomach's contents to flow up into the esophagus.
The severity of gerd depends on les dysfunction as well as the type and amount of fluid brought up from the stomach and the neutralizing effect of saliva.
What is the role of hiatial hernia in gerd?
Some doctors believe a hiatal hernia may weaken the les and increase the risk for gastroesophageal reflux. Hiatal hernia occurs when the upper part of the stomach moves up into the chest through a small opening. Many people with a hiatal hernia will not have problems with heartburn or reflux. But having a hiatal hernia may allow stomach contents to reflux more easily into the esophagus.
Coughing, vomiting, straining, or sudden physical exertion can cause increased pressure in the abdomen resulting in hiatal hernia. Obesity and pregnancy also contribute to this condition. Many otherwise healthy people age 50 and over have a small hiatal hernia. Although considered a condition of middle age, hiatal hernias affect people of all ages.
Hiatal hernias usually do not require treatment. However, treatment may be necessary if the hernia is in danger of becoming strangulated (twisted in a way that cuts off blood supply, called a paraesophageal hernia) or is complicated by severe gerd or esophagitis (inflammation of the esophagus). The doctor may perform surgery to reduce the size of the hernia or to prevent strangulation.
What other factors contribute to gerd?
Dietary and lifestyle choices may contribute to gerd. Certain foods and beverages, including chocolate, peppermint, fried or fatty foods, coffee, or alcoholic beverages, may trigger reflux and heartburn. Studies show that cigarette smoking relaxes the les. Obesity and pregnancy can also play a role in gerd symptoms.
What are the symptoms of heartburn?
Heartburn, also called acid indigestion, is the most common symptom of gerd and usually feels like a burning chest pain beginning behind the breastbone and moving upward to the neck and throat. Many people say it feels like food is coming back into the mouth leaving an acid or bitter taste.
The burning, pressure, or pain of heartburn can last as long as 2 hours and is often worse after eating. Lying down or bending over can also result in heartburn. Many people obtain relief by standing upright or by taking an antacid that clears acid out of the esophagus.
Heartburn pain can be mistaken for the pain associated with heart disease or a heart attack, but there are differences. Exercise may aggravate pain resulting from heart disease, and rest may relieve the pain. Heartburn pain is less likely to be associated with physical activity.
How common is heartburn and gerd?
More than 60 million adults experience heartburn at least once a month, and more than 15 million adults suffer daily from heartburn. Many pregnant women experience daily heartburn. Recent studies show that gerd in infants and children is more common than previously recognized and may produce recurrent vomiting, coughing, and other respiratory problems.
What is the treatment for gerd?
We recommend lifestyle and dietary changes for most people needing treatment for gerd. Treatment aims at decreasing the amount of reflux or reducing damage to the lining of the esophagus from refluxed materials.
Avoiding foods and beverages that can weaken the les is often recommended. These foods include chocolate, peppermint, fatty foods, coffee, and alcoholic beverages. Foods and beverages that can irritate a damaged esophageal lining, such as citrus fruits and juices, tomato products, and pepper, should also be avoided if they cause symptoms.
Decreasing the size of portions at mealtime may also help control symptoms. Eating meals at least 2 to 3 hours before bedtime may lessen reflux by allowing the acid in the stomach to decrease and the stomach to empty partially. In addition, being overweight often worsens symptoms. Many overweight people find relief when they lose weight.
Cigarette smoking weakens the les. Stopping smoking is important to reduce gerd symptoms.
Elevating the head of the bed on 6-inch blocks or sleeping on a specially designed wedge reduces heartburn by allowing gravity to minimize reflux of stomach contents into the esophagus. Do not use pillows to prop yourself up; that only increases pressure on the stomach.
Along with lifestyle and diet changes, doctor may recommend over-the-counter or prescription treatments.
Antacids can help neutralize acid in the esophagus and stomach and stop heartburn. Many people find that nonprescription antacids provide temporary or partial relief. An antacid combined with a foaming agent helps some people. These compounds are believed to form a foam barrier on top of the stomach that prevents acid reflux from occurring.
Long-term use of antacids, however, can result in side effects, including diarrhea, altered calciummetabolism (a change in the way the body breaks down and uses calcium), and buildup of magnesium in the body. Too much magnesium can be serious for patients with kidney disease. If antacids are needed for more than 2 weeks, a doctor should be consulted.
For chronic reflux and heartburn, the doctor may recommend medications to
Reduce acid in the stomach. These medicines include h2 blockers, which inhibit acid secretion in the stomach.
What if heartburn or gerd symptoms persist?
People with severe, chronic esophageal reflux or with symptoms not relieved by the treatments described above may need more complete diagnostic evaluation. Doctors use a variety of tests and procedures to examine a patient with chronic heartburn.
An upper gi series may be performed during the early phase of testing. This test is a special x-ray that shows the esophagus, stomach, and duodenum (the upper part of the small intestine). While an upper gi series provides limited information about possible reflux, it is used to help rule out other diagnoses, such as peptic ulcers.
Endoscopy is an important procedure for individuals with chronic gerd. By placing a small lighted tube with a tiny video camera on the end (endoscope) into the esophagus, the doctor may see inflammation or irritation of the tissue lining the esophagus (esophagitis). If the findings of the endoscopy are abnormal or questionable, biopsy (removing a small sample of tissue) from the lining of the esophagus may be helpful.
Esophageal manometric and impedance studies -- pressure measurements of the esophagus -- occasionally help identify low pressure in the les or abnormalities in esophageal muscle contraction.
For patients in whom diagnosis is difficult, doctors may measure the acid levels inside the esophagus through ph testing. Testing ph monitors the acidity level of the esophagus and symptoms during meals, activity, and sleep. Newer techniques of long-term ph monitoring are improving diagnostic capability in this area.
Does gerd require surgery?
A small number of people with gerd may need surgery because of severe reflux and poor response to medical treatment. However, surgery should not be considered until all other measures have been tried. Fundoplication is a surgical procedure that increases pressure in the lower esophagus. Endoscopic procedures that involve making the les function better or using electrodes to promote scarring of the les are newer options in treatment.
What are the complications of long-term gerd?
Sometimes gerd results in serious complications. Esophagitis can occur as a result of too much stomach acid in the esophagus. Esophagitis may cause esophageal bleeding or ulcers. In addition, a narrowing or stricture of the esophagus may occur from chronic scarring. Some people develop a condition known as barrett's esophagus. This condition can increase the risk of esophageal cancer.
Although gerd can limit daily activities and productivity, it is rarely life-threatening. With an understanding of the causes and proper treatment, most people will find relief.




+1.svg)
