Sinusitis: Management and Prevention
Sinusitis: Management and Prevention
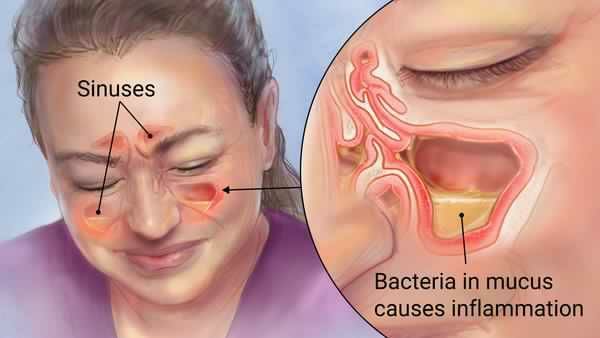
Sinusitis is infl ammation of the mucous membranes lining one or more of the paranasal sinuses. The various presentations are as folllows:
● acute sinusitis: infection lasting less than 30 days, with complete resolution of symptoms
● subacute infection: lasts from 30 to 90 days, with complete resolution of symptoms
● recurrent acute infection: episodes of acute infection lasting less than 30 days, with resolution of symptoms, which
Recur at intervals of at least 10 days apart
● chronic sinusitis: infl ammation lasting more than 90 days, with persistent upper respiratory symptoms
● acute bacterial sinusitis superimposed on chronic sinusitis:
New symptoms that occur in patients with residual symptoms from prior infection (s). With treatment, the new symptoms resolve but the residual ones do not.
Physical findings and clinical presentation
● patients often give a history of a recent upper respiratory illness with some improvement, then a relapse.
● mucopurulent secretions in the nasal passage
● purulent nasal and postnasal discharge lasting more than 7 to 10 days
● facial tightness, pressure, or pain
● nasal obstruction
● headache
● decreased sense of smell
● purulent pharyngeal secretions, brought up with cough, often worse at night
● erythema, swelling, and tenderness over the infected sinus in a small proportion of patients
● diagnosis cannot be excluded by the absence of such findings.
● these fi ndings are not common, and do not correlate with number of positive sinus aspirates.
● intermittent low-grade fever in about one half of adults with acute bacterial sinusitis
● toothache is a common complaint when the maxillary sinus is involved.
● periorbital cellulitis and excessive tearing with ethmoid sinusitis
● orbital extension of infection: chemosis, proptosis, impaired extraocular movements.
Characteristics of acute sinusitis in children with upper respiratory tract infections:
● persistence of symptoms
● cough
● bad breath
● symptoms of chronic sinusitis (may or may not be present)
● nasal or postnasal discharge
● fever
● facial pain or pressure
● headache
● nosocomial sinusitis is typically seen in patients with nasogastric tubes or nasotracheal intubation.
Cause
● each of the four paranasal sinuses is connected to the nasal cavity by narrow tubes (ostia), 1 to 3 mm in diameter; these drain directly into the nose through the turbinates. The sinuses are lined with a ciliated mucous membrane (mucoperiosteum).
● acute viral infection
● infection with the common cold or infl uenza
● mucosal edema and sinus infl ammation
● decreased drainage of thick secretions, obstruction of the sinus ostia
● subsequent entrapment of bacteria
A. Multiplication of bacteria
B. Secondary bacterial infection
Other predisposing factors
● tumors
● polyps
● foreign bodies
● congenital choanal atresia
● other entities that cause obstruction of sinus drainage
● allergies
● asthma
● dental infections lead to maxillary sinusitis.
● viruses recovered alone or in combination with bacteria (in 16% of cases):
● rhinovirus
● coronavirus
● adenovirus
● parainfluenza virus
● respiratory syncytial virus
● the principal bacterial pathogens in sinusitis are streptococcus pneumoniae, nontypeable haemophilus influenzae, and moraxella catarrhalis.
● in the remainder of cases, fi ndings include streptococcus pyogenes, staphylococcus aureus, alpha-hemolytic streptococci, and mixed anaerobic infections (peptostreptococcus, fusobacterium, bacteroides, prevotella).
Infection is polymicrobial in about one third of cases.
● anaerobic infections seen more often in cases of chronic sinusitis and in cases associated with dental infection; anaerobes are unlikely pathogens in sinusitis in children.
● fungal pathogens are isolated with increasing frequency in immunocompromised patients but remain uncommon
Pathogens in the paranasal sinuses. Fungal pathogens include aspergillus, pseudallescheria, sporothrix, phaeohyphomycoses, zygomycetes.
● nosocomial infections occur in patients with nasogastric tubes, nasotracheal intubation, cystic fi brosis, or those who are immunocompromised.
● s. Aureus
● pseudomonas aeruginosa
● klebsiella pneumoniae
● enterobacter spp.
● proteus mirabilis
Organisms typically isolated in chronic sinusitis:
● s. Aureus
● s. Pneumoniae
● h. Infl uenzae
● p. Aeruginosa
● anaerobes
Differential diagnosis
● migraine headache
● cluster headache
● dental infection
● trigeminal neuralgia
Workup
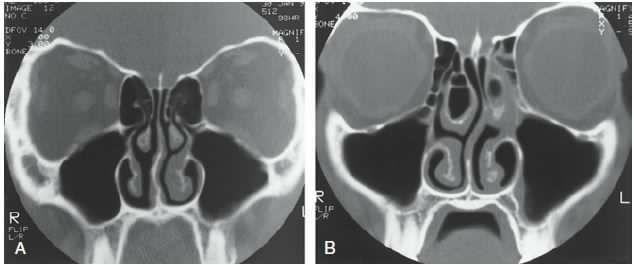
● water’s projection: sinus radiograph
● ct scan
● much more sensitive than plain radiographs in detecting acute changes and disease in the sinuses
● recommended for patients requiring surgical intervention, including sinus aspiration; it is a useful adjunct to
Guide therapy:
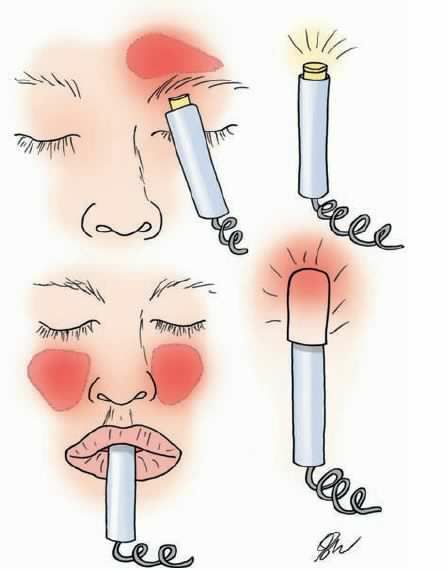
● transillumination
● used for diagnosis of frontal and maxillary sinusitis
● place transilluminator in the mouth or against cheek to assess maxillary sinuses, and under the medial aspect of the supraorbital ridge to assess frontal sinuses.
● absence of light transmission indicates that sinus is filled with fluid.
● dullness (decreased light transmission) is less helpful in diagnosing infection.
● endoscopy
● used to visualize secretions coming from the ostia of infected sinuses
● culture collection via endoscopy often contaminated by nasal flora; not nearly as good as sinus puncture
● sinus puncture
● gold standard for collecting sinus cultures
● generally reserved for treatment failures, suspected intracranial extension, nosocomial sinusitis.
Treatment Nonpharmacologic therapy
● sinus drainage
● nasal vasoconstrictors, such as phenylephrine nose drops, 0.25% or 0.5%
● topical decongestants should not be used for more than a few days because of the risk of rebound congestion.
● systemic decongestants
● nasal or systemic corticosteroids, such as nasal beclomethasone, short-course oral prednisone
● nasal irrigation, with hypertonic or normal saline (saline may act as a mild vasoconstrictor of nasal blood fl ow)
● use of antihistamines has no proved benefi t, and the drying effect on the mucous membranes may cause crusting,
Which blocks the ostia, thus interfering with sinus drainage.
● analgesics, antipyretics.
Antimicrobial therapy
● most cases of acute sinusitis have a viral cause and will resolve within 2 weeks without antibiotics.
● current treatment recommendations favor symptomatic treatment for those with mild symptoms.
● antibiotics should be reserved for those with moderate to severe symptoms who meet the criteria for diagnosis of
Bacterial sinusitis.
● antibiotic therapy is usually empirical, targeting the common pathogens.
● first-line antibiotics include amoxicillin, tmp-smz.
● second-line antibiotics include clarithromycin, azithromycin, amoxicillin-clavulanate, cefuroxime axetil, loracarbef, ciprofloxacin, levofloxacin.
● for patients with uncomplicated acute sinusitis, the less expensive first-line agents appear to be as effective as the
Costlier second-line agents.
Surgery
● surgical drainage indicated
● if intracranial or orbital complications suspected
● for many cases of frontal and sphenoid sinusitis
● for chronic sinusitis recalcitrant to medical therapy
● surgical débridement imperative for treatment of fungal sinusitis




+1.svg)
