Male Reproductive System (Human Anatomy): Image, Functions, Diseases, and Treatments
Last Updated: Feb 18, 2023
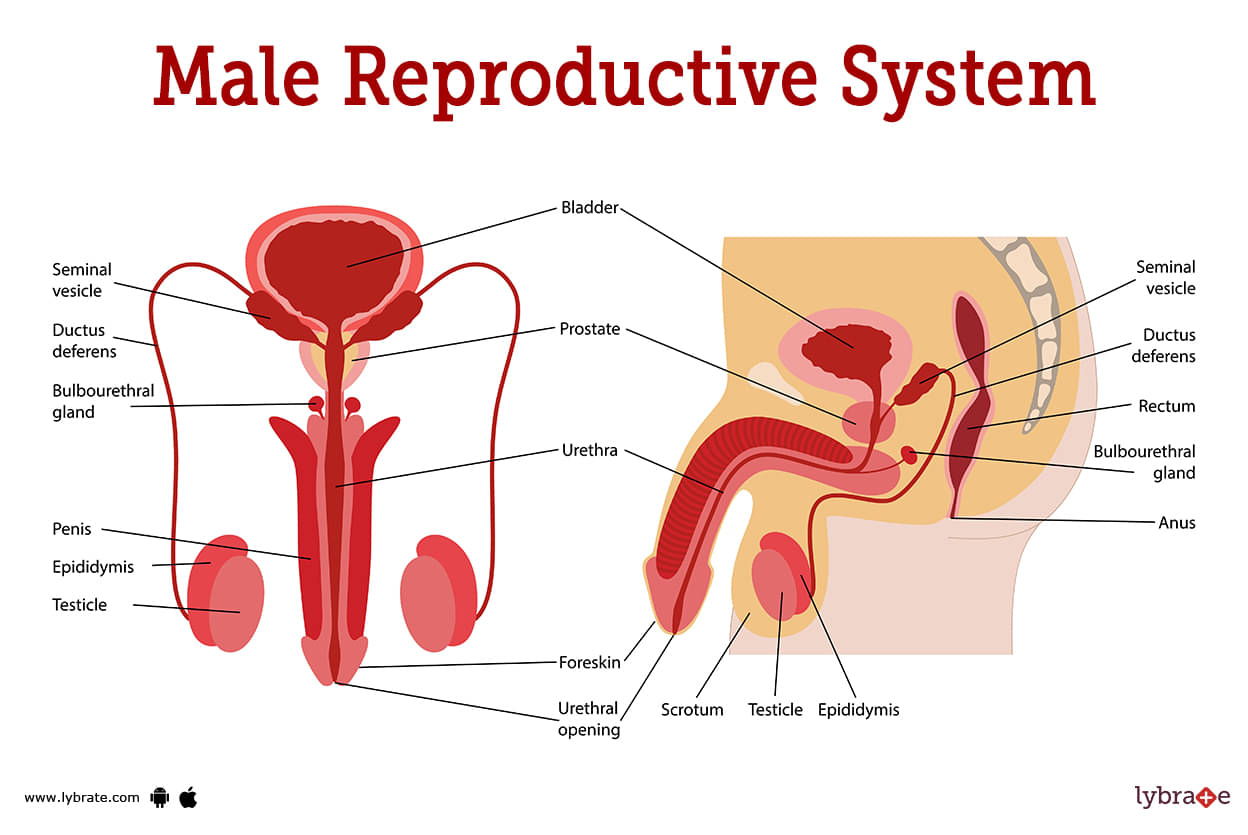
Male Reproductive System Image
Outside of the body is where you'll find most of male reproductive organs. The scrotum, the penis, and the testicles are all external organs. The urethra, the prostate, and the vas deferens are all internal organs. It's all in the male reproductive system, which regulates both urination and sexual activity.
Because humans are sexual, reproduction requires both a male and a female. Each is equipped with unique organs capable of making the cells required for reproduction.
Sexual intercourse, in conjunction with a woman's reproductive organs, has the ability to result in the reproduction of human life.
Males' external reproductive organs include:
- Penis: When stimulated, this tubular, muscular organ fills with blood, allowing for sexual contact.
- Scrotum: The scrotum is a pouch-like sac that hangs behind the penis and houses the testes, often known as testicles.
- Testicles: The testicles are two oval-shaped structures that create sperm and testosterone in the body.
Male Reproductive System Functions
Despite the fact that all males are born with all of their sexual organs, they do not begin to function normally until puberty. Around the age of 12, males begin puberty. During this era, hormonal changes affect a boy's gonads, resulting in long-term changes that have historically been regarded as 'when a boy becomes a man.' This process has various consequences, including greater height, muscular development, and genital and facial hair growth. At puberty, the sperm and sperm sacs of male become fully developed, making him fertile.
Spermatozoa, or sperm, are expelled from the testes of a man at the sexual climax. When this happens, it's termed 'ejaculating.' In order for fertilisation to take place, sperm must make their way to the female reproductive system, where they will get vital nutrients and be transferred to the egg.One ejaculate may contain as many as 750 million sperm cells, however, it takes only one viable sperm cell to fertilise an egg.
Natural hormone testosterone is delivered into the bloodstream immediately after being produced by the testes. Aside from controlling sperm production and keeping sexual function stable, testosterone also encourages secondary sex traits like facial hair, a deeper voice, increased muscle mass, and wider shoulders.
Male Reproductive System Conditions
- Obstruction of prostatic urethra: BPH often affects the median lobe, compressing the prostatic urethra and restricting urine flow. When the uvula vesicae become enlarged due to an expanded median lobe, a post-prostatic pouch of stagnant urine occurs behind the internal urethral opening. B.P.H. causes trouble urinating.
- Prostatic Carcinoma: Prostatic carcinoma symptoms include pain in the perineum, difficulty peeing, and blockage of the urinary system in the back. The levels of PSA and acid phosphatase in a patient's blood are two of the most important parameters to consider while detecting and treating prostate cancer.
- Hematuria: General Hematuria is caused by prostate damage, but it can also be caused by prostate infection.
- Urinary Incontinence: Urinary incontinence can result from an enlarged prostate or an infected prostate that blocks the urethral canal.
- Bacterial Prostatitis: Prostatitis caused by bacteria is called acute prostatitis and often affects younger men. Infections caused by E. coli, gonorrhoea, and chlamydia are the most prevalent causes of this condition.
- Prostatic Abscess: Abscesses in the prostate are caused by bacteria. Frequent urination, urinary pain, urinary retention, and urinary retention are all common symptoms.
- Prostatic Calculus: Microscopic stones that form in the prostate and have a brownish grey colour are called calculi. You may have heard of these stones in the prostate under that name. Prostate calculi can be either endogenous (originating in the prostate) or exogenous (originating outside of the prostate).
- Hydrocele: Fluid accumulation in the vaginal tunica (hydrocele) is the defining feature of this condition. While inflammation of the testicles may produce a hydrocele due to the tunica vaginalis' close proximity to the organ, idiopathic factors account for the great majority of hydroceles. Fluid from the tunica vaginalis can be drained by initially inserting a tiny trocar and then a cannula through the skin of the scrotal area.
- Varicocele: Simply described, varicocele is a medical condition in which the veins of the pampiniform plexus expand, get more tangled, and lengthen. The technical word for this condition is a varicocele. The vast majority of persons in this demographic (teens and young adults) experience this condition. The left side's higher incidence rate may be explained if we take into account the following.
- Tumours of the testis: The most frequent kind of testicular tumour is seminoma, sometimes called cancer of the seminiferous tubules; teratoma is the second most prevalent form of testicular tumour.
- Torsion of the testis: When the spermatic cord becomes twisted inside the scrotum, this is known as a torsion of the testis. This causes the testis to become deformed. Young people and physically active children are particularly vulnerable to this illness, which is characterised by excruciating pain.
- Cryptorchidism (incomplete descent of testis): During normal development, the testis should descend to the base of the scrotum. If it does not, a condition known as cryptorchidism will occur.
- Ectopic testis (maldescent of the testis): When one or both of a man's testicles are located at an abnormal location outside of the scrotum, a condition known as maldescent of the testis or ectopic testis has occurred.
- Scrotal edema: The skin is thin and the scrotum is in a dependent posture, therefore edoema is typical in that area.
- Sebaceous cysts: The scrotum has a lot of hair and sebaceous glands, thus this region of skin often gets clogged up with sebaceous cysts. This explains why scrotal skin is so prone to developing sebaceous cysts.
- Scrotal elephantiasis: Scrotal elephantiasis is a medical condition characterised by abnormal and extreme enlargement of the scrotum. Filariasis is characterised by a significant expansion and swelling of the scrotum because interstitial fluid that typically circulates in the scrotal wall collects there due to the obstruction of lymph arteries by the thin worms that cause filariasis (Wuchereria bancrofti).
- Orchitis: Swollen or inflamed testicles might be a sign of orchitis, a medical illness. Orchitis, like its close relative epididymitis, is typically brought on by a sexually transmitted infection (STD). Reduced sperm count, discomfort, swelling, fever, nausea, and vomiting are all symptoms of orchitis.
- Hypogonadism: Hypogonadism occurs when the body does not produce enough testosterone. It's possible that your brain isn't sending the right signals to your testicles to start producing hormones, or that your testicles themselves are malfunctioning.
- Testicular cancer: Testicular cancer affects thousands of American males over 18 each year. The low survival rate, and high cure rate for testicular cancer. This rare tumour affects young guys. Testicular cancer symptoms include a non-painful testicular tumour. Back pain, scrotum heaviness, groin soreness, and fatigue are frequent complaints.
- Spermatocele: A spermatocele can occur in the epididymis, a tiny, coiled tube that collects and transports sperm. In the epididymis, a spermatocele arises. Spermatoceles are harmless, non-spreading malignant growths. Milky or translucent fluid may include sperm.
- Contralateral testicular cancer: Metachronous contralateral testicular tumours are more common in patients with TGCT (CLTT). TGCT patients had a 15-fold greater risk of CLTT than the general population. The risk is double after a seminoma than after NSGCT, but it reduces with each treatment round. High-risk people should monitor their health.
- Fournier's gangrene: Fournier's gangrene is a lethal bacterial infection of the perineum, scrotum, or penis. This illness spreads quickly and requires immediate treatment.
- Testicular feminization syndrome: Testicular feminization syndrome. Androgen insensitivity syndrome (AIS) is a hereditary guy's resistance to male hormones like testosterone. This person has feminine physical characteristics yet male genes.
Male Reproductive System Test
- Physical Exam: Physically assess the patient A physical exam may help find lumps, swelling, or other testicular abnormalities. This may need palpation (the light touching of tissues). Your doctor may also move your leg, pelvis, or torso to check for testicular discomfort or abnormal movement. This method may diagnose testicular torsion.
- Ultrasound: Ultrasounds are commonly used to test parts of the male reproductive system. Noninvasive ultrasound scans the penis, scrotum, and other organs of the body for abnormalities. Abnormal blood flow can also identify testicular torsion, malignancy, and varicocele.
- Magnetic resonance imaging: MRI provides clear images of organs and tissues using powerful magnetic fields and radio waves. MRI is used to diagnose several reproductive problems (MRI). It helps doctors distinguish malignant from benign tumours.
- C.T. (Computed Tomography): A computed tomography (CT) scan combines x-ray and computer technologies to help in diagnosis. It can shoot from several angles. The computer combines them into a 3D picture.
- Blood test: various certain blood tests to search for specific proteins. These proteins, known as tumour markers, can help diagnose testicular cancer and also various markers for carcinoma in the reproductive system.
- X-ray: They will be able to detect irregularities that might suggest cancer using the examination images. These techniques can detect cysts, tumors, and torsions.
- Testicular Biopsy: A testicular biopsy has numerous possible applications, including obtaining sperm for in vitro fertilisation and diagnosing the reason of male infertility. A biopsy can identify the exact location and health of a testicular tumour (IVF).
- P.C.R: Polymerase Chain Reaction (or P.C.R. for short) is a method for determining which bacteria are responsible for male copulatory organ damage.
- Microscopic examination: Microscopical examination is one method for identifying infectious conditions such as bacterial infection.
Male Reproductive System Treatment
- Chemotherapy: Chemotherapy, sometimes known as chemotherapy, is a cancer treatment approach that involves the regular administration of one or more anti-cancer medications. Chemotherapy can be used for a variety of purposes, including illness cure, life extension, and symptom relief.
- Hormone treatment: Human chorionic gonadotropin, or hCG, is a peptide hormone that can be injected subcutaneously or intramuscularly as part of hormonal treatment (HCG). Because the success rate of hormone treatment is so low in comparison to surgical techniques, it should only be used as a last option.
- Orchiopexy: Orchiopexy, the most frequent procedure for a single descending testicle, has a nearly 100% success rate. Fertility rates are average for males with one undescended testicle but drop to 65% with two. Surgery can lessen testicular cancer risk, but it won't cure it.
Male Reproductive System Medicines
- Steroids for reducing inflammation of Male Reproductive System: For children, conservative therapy, which comprises applying steroidal cream for four to six weeks, is suggested.
- Phosphodiesterase inhibitors: The most commonly recommended drugs for people suffering from erectile dysfunction include sildenafil, vardenafil, tadalafil, and avanafil (ED).
- Analgesics for pain in Male Reproductive System: treatment for Penile Fracture, Ibuprofen may help reduce swelling and pain associated with this condition. In contrast, surgery and home care are the most helpful approaches to treating this condition.
- Antibiotics for infection in Male Reproductive System: Antibiotics and painkillers are commonly given together to patients who have been diagnosed with urethritis. Azithromycin (Zithromax), doxycycline coupled with ceftriaxone (Rocephin), and cefixime are common antibiotics used to treat this condition (Suprax).
- Antifungals for treating infection of Male Reproductive System: Treatment for balanoposthitis often entails the use of antifungal medications such as clotrimazole, metronidazole, or miconazole. There are additional cases where miconazole is utilised.
- Chemotherapeutic medicines for Male Reproductive System: Cancer patients may benefit from chemotherapy, which includes As part of the treatment for sarcoma or other malignancies of the calf muscle, chemotherapy or other anti-cancer medications may be provided to the patient. This contributes to the maximum efficiency in curing the ailment.
Frequently Asked Questions (FAQs)
What is the most common male reproductive infection?
Can most male infertility be treated?
How can I treat male infertility at home?
How can male fertility be improved?
What is the problem of the male reproductive system?
What causes infection in the male reproductive system?
What are the causes of reproductive diseases?
Can male fertility be cured?
Table of content
Find Urologist near me
Ask a free question
Get FREE multiple opinions from Doctors