Plantar Fasciitis: Causes, Symptoms, Treatment and Cost
Last Updated: Jul 06, 2023
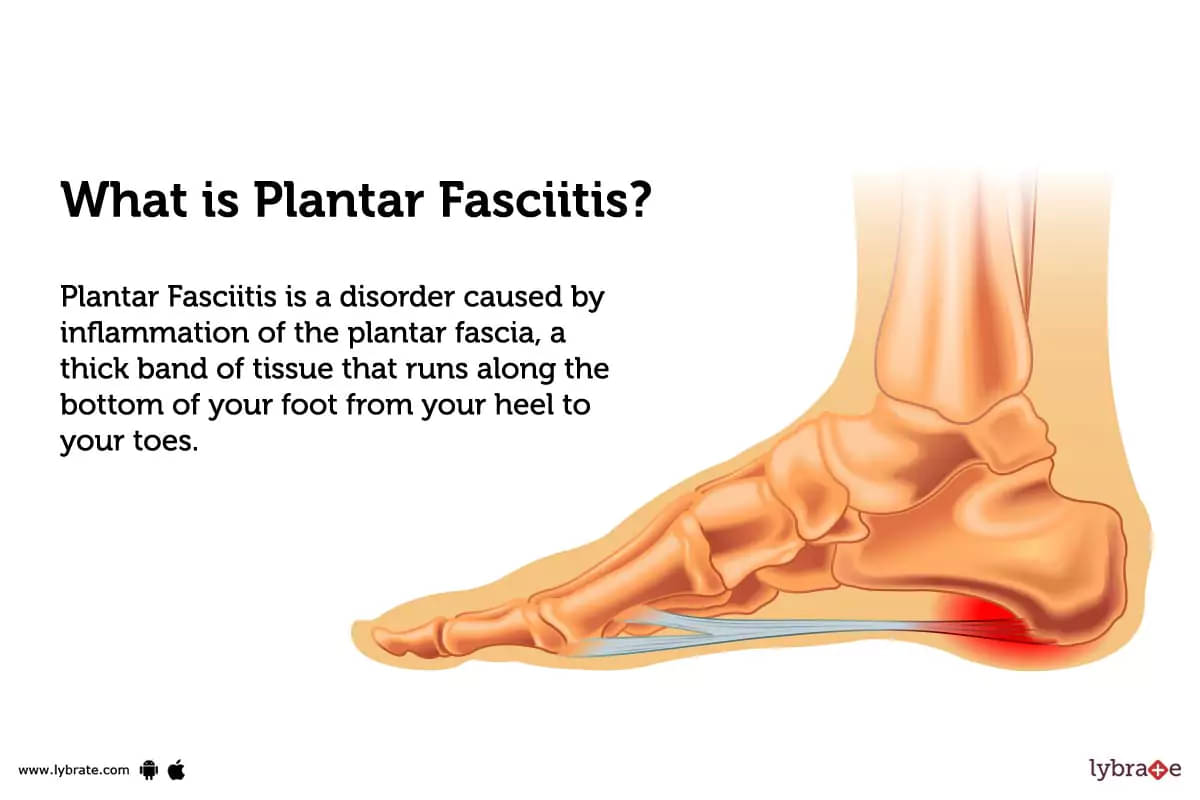
What is Plantar Fasciitis?
Plantar Fasciitis is a disorder caused by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot from your heel to your toes. It's also called a heel spur - a bony protrusion on the bottom of your heel bone.
Types of Plantar Fasciitis
There are two main types of plantar fasciitis: insertional plantar fasciitis and non insertional plantar fasciitis.
- Insertional Plantar Fasciitis: It occurs when the tissue at the base of your heel that connects to your tendons and ligaments experiences inflammation. This type commonly affects adults over 40 years old and is caused by repetitive strain injury or by extreme physical activity like running or jumping.
- Non insertional Plantar Fasciitis: It typically occurs when too much tension is placed on tight calf muscles, which pull on your Achilles tendon, overstretching it until it causes microtrauma in your plantar fascia tissue near where it attaches to your heel bone. This type tends to occur in people under 40 years old who are physically active and generally affects one foot more than the other.
What causes Plantar Fasciitis?
- Some of the most common causes of plantar fasciitis include:
- Excessive running or other high-impact activities.
- Wearing badly fitting shoes that don’t support and cushion your feet.
- Obesity
- Jobs that require you to stand on hard surfaces for long periods of time.
- Additionally, having conditions such as flat feet or an abnormal gait can increase your risk of developing this painful condition.
What are the symptoms of Plantar Fasciitis?
- Pain and discomfort in the heel and/or arch area of the foot.
- Pain upon rising or taking your first steps after sleeping.
- Sharp or stabbing pain that usually subsides after walking around for a few minutes, but reappears with activity or long periods of standing or sitting.
- Tenderness and swelling in the heel area with possible bruising on the sole of the foot.
How can you prevent Plantar Fasciitis?
- Wear supportive, cushion shoes with good arch support.
- Perform foot exercises to strengthen feet and arches.
- Avoid walking barefoot and activities that may strain the plantar fascia.
- Stretch feet, lower legs, and calf muscles regularly.
- Place a night splint or brace to keep feet in dorsiflexion while sleeping.
- Control existing medical conditions that may increase risk of developing Plantar Fasciitis, such as overweight/obesity and diabetes.
- Use shock absorbing insoles/orthotics for additional arch support where necessary.
Plantar Fasciitis - Diagnosis and Tests
- Physical exam: The physical exam for plantar fasciitis will involve testing the range of motion in the ankle and foot, palpating the foot and arch, and testing motor strength in the legs. The doctor may also check for any inflammation of the tissues surrounding the heel and arch, as well as signs of nerve damage.
- X-rays: X-rays are typically used to diagnose plantar fasciitis. This type of imaging will show any signs of bone spurring or calcium deposits in the foot. Additionally, it might assist in ruling out other reasons for your heel pain, such as stress fractures, arthritis, or nerve problems.
- Ultrasound: Ultrasound imaging can be a helpful adjunct in diagnosing plantar fasciitis. Ultrasound imaging can detect swelling or inflammation of the plantar fascia, detect abnormalities of the structure, and identify sites of origin or insertion.
- Magnetic resonance imaging (MRI): A powerful magnetic field and radiofrequency waves are used in the imaging process known as magnetic resonance imaging (MRI) to provide precise pictures of the inside of the body. MRI may be recommended for evaluating plantar fasciitis, as it can provide clear images of the feet, as well as any associated signs of inflammation, such as heel spur formation.
- Computed tomography (CT) scans: Computed tomography (CT) scans provide a highly detailed look at the anatomy of the foot and ankle, allowing for accurate diagnosis of plantar fasciitis. Depending on the severity of the condition, CT scans can be used to detect any areas of calcification or scarring, as well as any bony abnormalities.
What are possible complications of Plantar Fasciitis?
- Ongoing Foot Pain: Plantar fasciitis can cause persistent foot pain, even impairing daily activities.
- Heel Spurs: Heel spurs may develop as a result of the ailment if it is left untreated.
- Reduced Mobility: Sufferers may experience limited mobility and reduced flexibility in their toes and feet.
- Loss of Strength: Over time, the plantar fascia fibres may begin to wear down, leading to a loss of strength in the foot muscles and tendons.
- Nerve Damage: Chronic plantar fasciitis can cause nerve damage and inflammation in the foot, which may lead to numbness or loss of feeling in certain areas of the foot or toes.
Home Remedies for Plantar Fasciitis?
- Drink ginger tea twice a day to reduce inflammation and pain associated with plantar fasciitis.
- Use foot icing every night before going to bed in order to reduce inflammation and pain related to plantar fasciitis.
- Massage your feet with an oil such as sesame or coconut oil, as this helps in relieving the calcified tissues causing pain in the feet.
- Apply warm castor oil compress many times a day for 5-10 minutes to improve circulation and reduce swelling of the ligament caused by plantar fasciitis.
What to eat in Plantar Fasciitis?
- Eat a balanced diet full of protein, calcium and Vitamin D to help reduce inflammation.
- Include foods packed with antioxidants in your diet, such as cherries, almonds, and oats, to boost your body's defences.
- Choose low-acid fruits and vegetables such as collards, celery and squash to prevent further tissue damage from acidity.
- Increase intake of omega-3 fatty acids found in salmon and other fatty fish for anti-inflammatory effects on the body.
What not to eat in Plantar Fasciitis?
- High fat, processed and fried foods: These can increase inflammation in the body, making the pain from plantar fasciitis worse.
- High amounts of salt and sugar: Excess salt and sugar can also impact inflammation, worsening foot pain.
- Certain dairy products: Dairy products like cheese and yoghourt can increase inflammation levels due to their high calcium content.
- Alcohol: Intoxicating beverages such as beer or wine should be avoided as they worsen foot pain.
Plantar Fasciitis Treatment
- Rest: To assist decrease inflammation and discomfort in the afflicted region, the first and most crucial step is to get some rest. Give yourself a break from activities that are hard on your feet and plantar fascia, such as running or jumping.
- Stretching: Stretches can help improve flexibility, decrease tension in the muscles,and increase circulation to the affected area. Examples of stretches include towel stretches,rolling on a frozen water bottle, or calf stretching using a wall or door frame.
- Orthotics: Custom orthotics are sometimes prescribed by a doctor to provide more arch support and cushioning for the foot to reduce strain on the plantar fascia.
- Endoscopic Plantar Fasciotomy: This involves the use of an endoscopic camera to make small incisions in the fascia and release tension.
- Open Release Surgery: This is a more invasive procedure, where an incision is made larger for more extensive release of tension in the plantar fascia.
- Heel Spur Removal: If a heel spur is aggravating symptoms, it may be removed as part of plantar fasciitis treatment.
- Shock Wave Therapy: High-energy sound waves are used to target inflamed areas of the ligament with varying degrees of success reported in clinical trials.
Which doctor to consult for Plantar Fasciitis?
A doctor that specialises in podiatry, or foot health, should be consulted for Plantar Fasciitis. This type of doctor can diagnose and treat the condition with a variety of methods and provide the best advice to the patient to get relief from the pain associated with it.
Which are the best medicines for Plantar Fasciitis?
- Non-steroidal anti-inflammatory drugs (NSAIDs): These are the medications that doctors most often recommend to treat plantar fasciitis in order to lessen the inflammation and pain associated with the condition. Examples include ibuprofen or naproxen.
- Corticosteroid injections: These injections may help decrease pain and inflammation in the impacted region, providing relief in the period while other therapies take effect.
How long does it take to recover from Plantar Fasciitis?
The recovery time for plantar fasciitis can depend on the severity of the condition, as well as other factors such as age, physical activity, and any additional foot conditions that may be present.
Generally speaking, a person with plantar fasciitis can take anywhere from several weeks to several months to fully recover.
What is the cost of Plantar Fasciitis treatments in India?
- The cost of Plantar Fasciitis treatments in India varies widely, depending on the severity of the condition and the types of treatments being sought.
- Medications for pain relief can range from over-the-counter medications to prescription narcotics; prices will vary accordingly.
- Physical therapy sessions start at around 2000 INR per session.
- Custom orthotics can range from 3000 to 8000 INR.
- Surgical procedures can cost up to 75000 INR or more.
What are side-effects of Plantar Fasciitis treatments?
- Common side effects of Plantar Fasciitis treatments can include heel pain and inflammation, swelling, muscle spasms, and stiffness that last for a few days after treatment.
- If the treatment is a particular procedure like steroid or platelet-rich plasma injections, possible side effects to look out for are infection at injection site or tendon rupture depending on procedure.
- Other possible side effects are nerve irritation, skin discoloration and excessive growth of bone in the foot due to overuse of the area that was treated with injections.
Plantar Fasciitis - Outlook/ Prognosis
If you are experiencing any plantar fasciitis problems, you should see a doctor in your area right away. These problems may lead to 'heel spurs, decreased mobility, and nerve damage,' for which the length of your treatment programme will depend on how severe your condition is.
Table of content
Find Sports Medicine near me
Ask a free question
Get FREE multiple opinions from Doctors