Sclera (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Mar 17, 2023
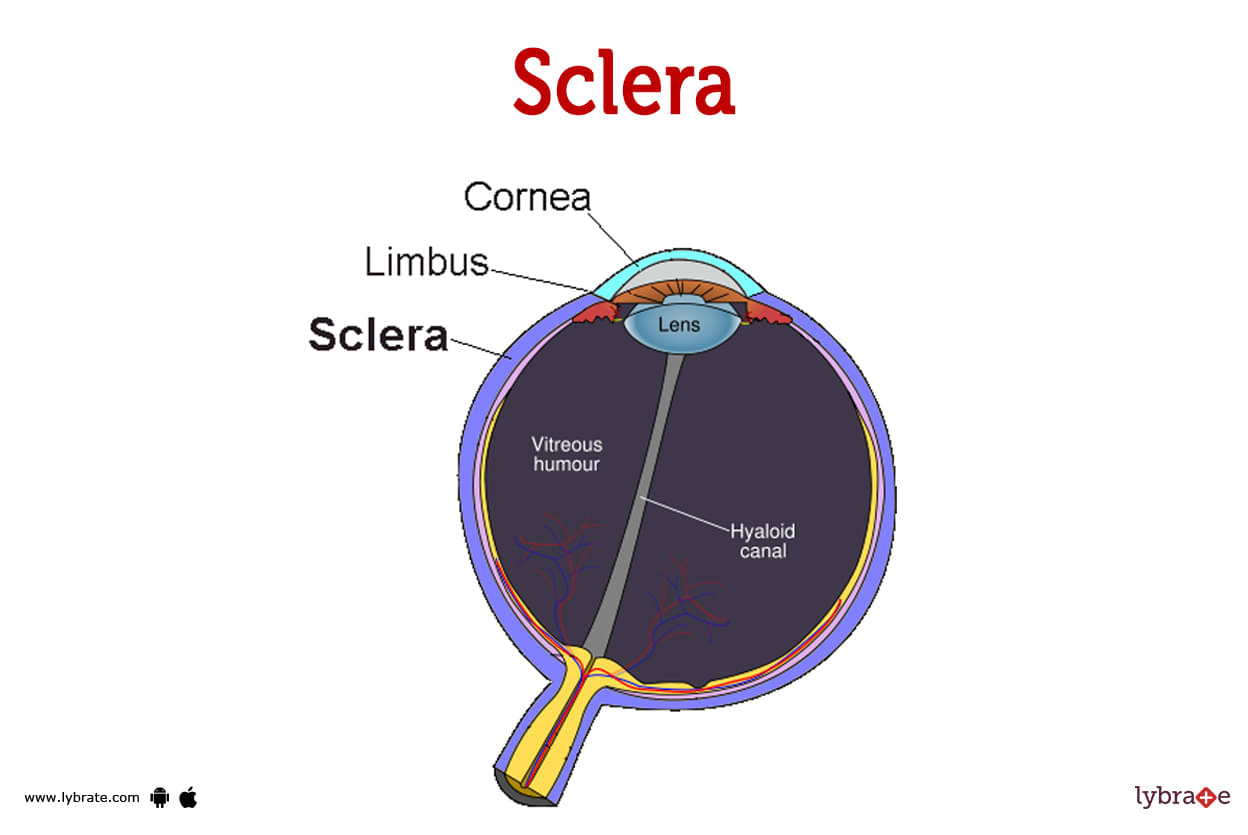
Sclera Image
The sclera, or white of the eye, is a thick tissue that encircles the eyeball. It helps keep the shape of your eyeball and protects it from damage. For a variety of reasons, the entire sclera may change colour or develop coloured patches. Not all scleral problems resolve on their own in a few weeks, but many do.The majority of the eyeball is protected by the sclera, sometimes known as the white of the eye. It reaches from the front cornea to the rear optic nerve.
Your eyeball's white appearance is due to a robust covering of tissue that is only a millimetre thick. Your eye is also supported and protected by it. Sclerae is the plural form of sclera.
What is the anatomy of the sclera?
Collagen fibres that are strong and crisscross randomly make up the sclera. Your eyeball's white colour and sclera strength come from that random pattern. The collagen fibres in your cornea, which are remarkably organised and enable the cornea to remain transparent, stand in contrast to this.
There are four layers that make up the sclera, arranged from outside to inside:
- Episclera: On top of the whites of your eyes lies a transparent, thin tissue called the episclera.
- Stroma: The stroma, which is made up of fibroblasts and collagen fibers, is mixed with the episclera.
- Lamina fusca: The lamina fusca is a layer that lies between both the sclera and also the choroid as well as ciliary body outer layers.
- Endothelium: The deepest or basal layer of the sclera is called the endothelium.
Sclera Functions
The sclera acts as a retaining wall for the eyeball. It helps keep the shape of your eyeball and guards against injury.
The sclera is covered by the conjunctiva, that are clear mucous membranes which lubricate (moisten) your eye. The sclera-attached muscles help move your eyeball up and down as well as side to side.
Sclera Conditions and Disorders
- Ectasia: When your eyeball is injured or inflamed, the conjunctiva may become thinner or thicker. You could need special glasses, or perhaps this will go away on its own.
- Episcleritis: Inflammation of the episclera (swells). Your eyes may be puffy, irritated, and red. The syndrome may be associated with an inflammatory condition, such rheumatoid arthritis. Episcleritis normally resolves on its own within a few weeks, however it sometimes recurs.
- Scleral coloboma: Occasionally, a piece of the sclera is absent at birth. As a consequence, your eyeball can develop a cleft or a protrusion. The kind of therapy employed depends on how severe the sickness is. Usually, it involves helping patients maintain good eye health and get the most out of their vision.
- Scleritis: Scleritis is more harmful and usually more painful than episcleritis, despite the similarities between the two. Searing eye discomfort brought on by scleritis is common and becomes worse when you move your eyes. It might cause long-lasting damage and vision loss.
- Sclera calcification: Senile scleral plaques may develop as a consequence of aging-related calcium deposits in the sclera. On your sclera, these plaques may show up as grey dots at just 3 and 9 o'clock. They very seldom irritate or infect the eye by penetrating the sclera surface.
- Scleromalacia perforans: Scleromalacia Anterior necrotizing scleritis without inflammation is known as perforans. often seen in females with protracted seropositive rheumatoid arthritis. In the absence of high intraocular pressure, spontaneous perforation is uncommon.
- Senile scleral plaques: Age-related calcium deposits in the sclera may result in senile scleral plaques. These plaques might show up as grey patches on your sclera at the 3 and 9 o'clock positions. They very seldom penetrate the conjunctival surface and irritate or infect the eye.
- Staphyloma(Ciliary staphyloma): The area of scleral ectasia houses the ciliary body. Scleritis, trauma, developing glaucoma, and end-stage primary/secondary glaucoma are among the causes.
Why isn't the sclera of my eye white?
Several things can cause the entire sclera to change colour or spots of colour to appear:
- Blue sclera: Your eyes may seem blue or grey if your sclera is thinner than usual and blood vessels may be seen through it. Some persons with certain medical issues may experience this. Examples include Marfan syndrome and the inherited bone disease osteogenesis imperfecta (a disorder in connective tissue throughout the body). Anaemia and iron deficiency are two further instances.
- Icteric sclera and jaundice: If the sclera completely becomes yellow, you may have jaundice. Jaundice is a sign of liver illness, which prevents the liver from adequately filtering blood.
- Injury: Your eyeball may have a stark red area if it is hurt. This is a sign of a blood vessel that has cracked and released some blood. These innocuous red patches normally disappear within a few days or weeks.
- Irritation: If ones eyes are 'bloodshot,' the sclerae will be red all over. Smoke, allergies, exhaustion, or an infection can all irritate the eyes.
- Medication: Certain drugs may cause the sclerae to become blue or grey (for example, an antibiotic called minocycline).
- Melanosis: There might be a brown, flat patch on your sclera that resembles a freckle. Black folks are more likely to experience this. The innocuous spots are brought on by an excess of a pigment called melanin.
- Pinguecula: Your sclera may develop a small yellow patch as a result of sun, wind, or dust damage. It's possible for the patch to swell up and turn pink or red.
- Pterygium: Untreated pingueculae may become bigger, enlarge into the cornea, and obstruct vision.
- Primary acquired melanosis (PAM): A flat brown patch that varies over time on the eye might be a sign of PAM. Any new or changing spots on the sclera should be reported since this disease might become malignant.
How long does it take for the sclera to heal?
Scleral irritation or minor injuries often subside within a few days or weeks. But if you have any other symptoms or the issue persists, see an ophthalmologist or member of your healthcare team. An ophthalmologist is an expert in conditions that affect the eyes.
How can I protect my sclerae?
- Several easy precautions can help shield your sclerae from harm like When practising sports or performing home repairs, put on safety goggles.
- Protect your eyes from wind, debris, and the sun by wearing sunglasses.
- To avoid spreading infection, wash your hands before touching your eyes.
Sclera Tests
- CBC: In order to ascertain if an infection or immunological issue is present, a complete blood count is performed.
- Microscopic Inspection: It is occasionally possible to remove scleral tissue and examine it on a microscope to look for modifications. To rule out highly contagious or cancerous causes, this is done.
- B-Scan Ultrasonography: The thickness of the sclera and choroid, the presence of scleral nodules, the accumulation of fluid in the Tenon's capsule, the separation of the retina, etc. are typical ultrasonographic findings of scleritis.
- Magnetic resonance imaging (MRI): By doing a circular MRI of the whole eye and seeing the sclera sheath, magnetic resonance imaging (MRI) may also assist in identifying posterior scleritis.
Sclera Treatments
- Scleritis surgical treatment: Scleritis does not commonly need surgical treatment. Scleral thinning may need the insertion of a scleral transplant. Minor corneal holes are treated with bandage contacts or corneal glue prior to having surgical surgery. Donor stroma, fascia lata, and sclera were acquired to reinforce the sclera.
- Conjunctivectomy: It is the repair of the sclera and conjunctiva utilising conjunctival autografting and amniotic membrane inlay filling, and to evaluate the clinical result the patients are assessed clinically.
- Keratoplasty: Replacement of damaged cornea by a graft of homologous tissue.
Sclera Medicines
- Steroids for treatment of inflammation fo sclera: Steroids for treating Sclera inflammation include: 50 mg indomethacin three times per day; 600 mg ibuprofen three times per day; and 500 mg naproxen twice per day.
- NSAIDS for pain in the sclera: In mild to severe instances of scleritis, analgesics for discomfort in the sclera (NSAIDs) are the first line of therapy. Selective or non-selective cyclo-oxygenase inhibitors, such as Indomethacin, Ibuprofen, or Flurbiprofen, may be used in the course of the therapy.
- Immunosuppressive drugs for treatment of necrotizing scleritis: drugs that are used to treat necrotizing scleritis; depending on the systemic illness, drugs such doxorubicin, misoprostol, sildenafil, and mycophenolate may be suggested. The dangerous condition necrotizing scleritis is treated with glucocorticoids and immunosuppressive drugs.
- Antibiotics for treatment of infection of sclera: Antibiotics are used to treat scleritis caused by bacterial infections, such as those caused by ciprofloxacin, moxifloxacin, and amoxicillin.
- Antifungal medicines for treatment of infection of sclera: If Sjogren's syndrome is the underlying cause of the scleritis, antifungal medications may be used to treat it. similar to voriconazole.
When should I call a healthcare professional?
If you notice any changes in your sclera, such as a decrease in your eyesight or hazy vision, you should get in touch with a healthcare professional as soon as possible.
- Bulging.
- The tint of your eyes' whites changes.
- A speck on the white of your eye that is already there changes (for example, it changes colour or gets larger).
- Discharge (fluid or pus seeping out of your eye) (fluid or pus leaking out of your eye)
- Injuries or soreness
- Light sensitivity.
- Swelling inside your eye.
Table of content
Find Ophthalmologist near me
Ask a free question
Get FREE multiple opinions from Doctors