Tonsil stones - Symptoms, Causes Treatments And Cost
Last Updated: May 10, 2023
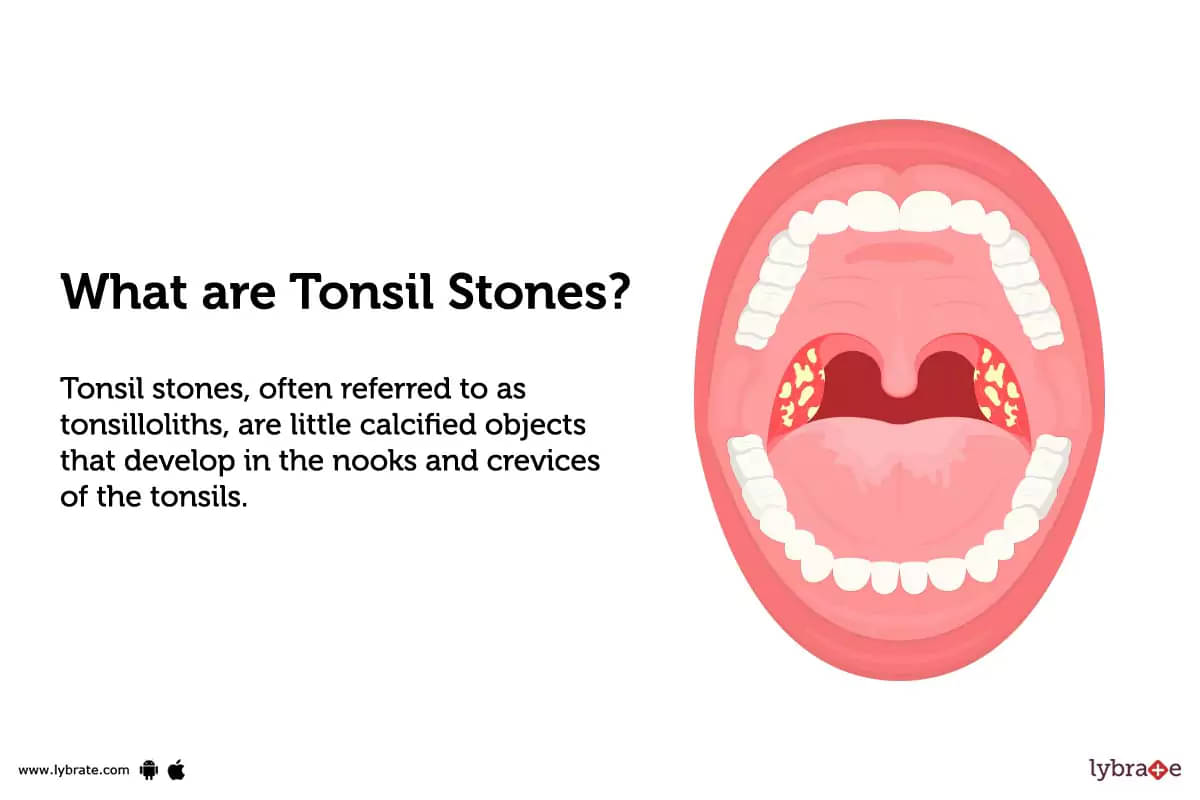
What are tonsil stones?
Tonsil stones, often referred to as tonsilloliths, are little calcified objects that develop in the nooks and crevices of the tonsils. These structures are typically composed of a mixture of dead cells, bacteria, and debris that become trapped in the tonsil crypts and calcify over time.
The formation of tonsil stones is a common occurrence and can be caused by a variety of factors, including poor oral hygiene, chronic tonsillitis, and the accumulation of food particles and other debris in the tonsil crypts.
What do tonsil stones look like?
Tonsil stones, also known as tonsilloliths, typically appear as small, white or yellowish, irregularly shaped lumps or clusters lodged in the pockets or crevices of the tonsils. They could be as little as sand grains or as big as pea-sized aggregates.
The appearance of tonsil stones can vary depending on their composition and the stage of development. Early-stage tonsil stones may resemble small, white or yellowish flecks or spots on the tonsils, while more advanced formations may appear as larger, solid masses that protrude from the tonsil surface.
It is important to note that the appearance of tonsil stones can vary from person to person.
What’s the difference between tonsil stones and tonsillitis?
Tonsil stones and tonsillitis are two distinct conditions that affect the tonsils, but they differ in their causes, symptoms, and treatments.
Tonsil stones, often referred to as tonsilloliths, are tiny calcified objects that develop in the nooks and crevices of the tonsils. They are typically composed of a mixture of dead cells, bacteria, and debris that become trapped in the tonsil crypts and calcify over time. Tonsil stones can cause unpleasant symptoms such as bad breath, sore throat, and difficulty swallowing, but are generally harmless.
Tonsillitis, on the other hand, is an infection or inflammation of the tonsils that is typically brought on by a viral or bacterial infection. Symptoms of tonsillitis may include sore throat, difficulty swallowing, fever, and swollen lymph nodes, among others.
What causes tonsil stones?
Tonsil stones, also known as tonsilloliths, are caused by a variety of factors related to the anatomy and function of the tonsils. These factors include;
- Trapped debris: The tonsils contain numerous crevices and pockets that can trap bacteria, dead cells, and other debris. Over time, these materials can accumulate and become calcified, leading to the formation of tonsil stones.
- Poor oral hygiene: Inadequate oral hygiene can contribute to the buildup of bacteria and debris in the mouth and throat, increasing the risk of tonsil stone formation.
- Chronic tonsillitis: Recurrent or persistent tonsillitis can cause inflammation and damage to the tonsil tissue, creating more crevices and pockets for debris to accumulate and leading to the formation of tonsil stones.
- Dry mouth: A dry mouth can contribute to the buildup of bacteria and debris in the mouth, increasing the likelihood of tonsil stone formation.
- Diet: Certain foods, such as dairy products, may contribute to the formation of tonsil stones by increasing mucus production and providing a source of nutrients for bacteria.
- Genetics: Some people may be more prone to tonsil stone formation due to inherited traits related to the structure and function of the tonsils.
What are the symptoms of tonsil stones?
Tonsil stones, also known as tonsilloliths, may produce a range of symptoms that can vary in severity depending on the size and location of the stones. Some common symptoms of tonsil stones include;
- Bad breath
- Sore throat
- Difficulty swallowing
- Ear pain
- Swollen tonsils
- White or yellowish spots on the tonsils
- Coughing
How are tonsil stones diagnosed?
Diagnosing tonsil stones, also known as tonsilloliths, typically involves a physical examination of the throat and tonsils, as well as a review of the patient's medical history and symptoms. Some common methods used to diagnose tonsil stones include;
- Visual inspection: A healthcare provider may use a lighted instrument to examine the throat and tonsils for the presence of tonsil stones. The stones may appear as small white or yellowish flecks or clusters on the surface of the tonsils.
- Palpation: In some cases, a healthcare provider may use gentle pressure to feel for the presence of tonsil stones within the tonsil crypts.
- Imaging tests: In rare cases, imaging tests such as X-rays, CT scans, or ultrasound may be used to visualize the tonsils and identify the presence of tonsil stones.
- Oral swabs: A healthcare provider may use a cotton swab or other instrument to collect a sample of the tonsil stones for further analysis or testing.
If a diagnosis of tonsil stones is confirmed, treatment may depend on the size and location of the stones, as well as the severity of any associated symptoms.
How are tonsil stones treated?
The treatment of tonsil stones, also known as tonsilloliths, can vary depending on the size and severity of the stones, as well as the associated symptoms. Some common methods used to treat tonsil stones include;
- Manual removal: In some cases, small tonsil stones can be removed manually with a cotton swab or other instrument. This is typically done in a healthcare provider's office under local anesthesia.
- Salt water gargles: Gargling with warm salt water may help to dislodge tonsil stones and reduce associated inflammation or irritation.
- Oral irrigators: Oral irrigators or water picks may be used to flush out tonsil stones from the tonsil crypts.
- Antibiotics: In some cases, tonsil stones may be accompanied by a bacterial infection. In order to treat the infection and lessen inflammation, antibiotics may be recommended.
- Tonsillectomy: In severe cases or cases where tonsil stones are causing persistent symptoms, a tonsillectomy may be recommended. This procedure, which involves surgically removing the tonsils, is normally saved for situations in which other treatments have failed.
Is there a way to remove tonsil stones surgically?
Yes, tonsillectomy surgery can be used to medically remove tonsil stones. During a tonsillectomy, the tonsils are completely removed from the back of the throat, which eliminates the tonsil crypts where tonsil stones can form. This procedure is typically reserved for cases where other treatments have been ineffective, and may be recommended for patients who experience frequent or severe tonsil stones, or who have other complications such as recurrent tonsillitis or difficulty swallowing.
How can I prevent tonsil stones?
While it is not always possible to completely prevent tonsil stones from forming, there are several measures that may reduce the risk of developing them or help to manage symptoms associated with tonsil stones. Some tips to help prevent tonsil stones include;
- Practice good oral hygiene: Brushing your teeth twice a day, flossing daily, and using an antiseptic mouthwash can help to reduce the amount of bacteria and debris that can accumulate in the tonsil crypts.
- Stay hydrated: Drinking plenty of water and other fluids can help to keep the mouth and throat moist, which may reduce the risk of tonsil stones forming.
- Avoid smoking or using tobacco products: Tobacco use can contribute to the development of tonsil stones by increasing bacterial growth and irritating the throat.
- Limit alcohol consumption: Drinking alcohol can also contribute to bacterial growth in the mouth and throat, which may increase the risk of tonsil stones.
- Use a waterpik or oral irrigator: These devices can help to flush out debris and bacteria from the tonsil crypts, reducing the risk of tonsil stone formation.
- Seek treatment for underlying conditions: Chronic sinus infections, postnasal drip, or gastroesophageal reflux disease (GERD) can all contribute to the development of tonsil stones. Seeking treatment for these conditions may help to reduce the risk of tonsil stone formation.
How do I take care of myself if I have tonsil stones?
There are numerous actions you may do to take care of yourself and control your symptoms if tonsil stones have been diagnosed. Some tips for self-care when dealing with tonsil stones include;
- Brush your teeth twice a day, floss daily, and use an antiseptic mouthwash to help reduce bacteria and debris in the mouth.
- Gargling with salt water might help to ease throat discomfort and reduce inflammation.
- Waterpik or oral irrigators can be helpful in dislodging tonsil stones and flushing out debris from the tonsil crypts.
- Tobacco products, alcohol, and spicy or acidic foods can all irritate the throat and exacerbate symptoms.
- Drinking plenty of water can help to keep the mouth and throat moist, which may reduce discomfort associated with tonsil stones.
- Over-the-counter pain relievers such as acetaminophen or ibuprofen may help to reduce pain and inflammation associated with tonsil stones.
- It's critical to contact a doctor if your tonsil stones persist or create excruciating pain. A healthcare provider may be able to recommend additional treatment options, such as surgical removal of the tonsils.
When should I see a healthcare provider about tonsil stones?
If you suspect you have tonsil stones, it is generally recommended to see a healthcare provider for diagnosis and treatment. However, there are specific circumstances where seeking medical attention is particularly important. Here are some pointers on when to see a healthcare provider about tonsil stones;
- If you are experiencing persistent or worsening symptoms such as bad breath, sore throat, or difficulty swallowing, it is important to seek medical attention.
- If your tonsil stones are particularly large or causing significant pain or discomfort, a healthcare provider may be able to recommend more aggressive treatment options.
- If you have a history of recurrent tonsil stones, it may be necessary to seek medical attention to discuss preventive measures or more long-term treatment options.
- While complications from tonsil stones are rare, they can occur. It is crucial to get medical assistance right away if you are worried about potential complications like an infection or respiratory problems.
- If you experience any unusual or concerning symptoms such as bleeding or a persistent lump or growth in the throat, it is important to seek medical attention promptly.
What doctor removes tonsil stones?
Tonsil stones can be removed by several healthcare professionals, depending on the severity and location of the stones. Most frequently, tonsil stones are removed by an otolaryngologist, also referred to as an ENT specialist. These doctors have specific education and experience in the diagnosis and treatment of tonsil stones and other disorders of the ears, nose, throat, and neck.
In some cases, a dentist or oral surgeon may also remove tonsil stones, particularly if they are located near the back of the mouth or in the tonsil crevices. Additionally, a primary care physician may be able to diagnose and treat mild cases of tonsil stones, but they may refer patients to an ENT specialist for more complex cases or recurrent tonsil stones.
How much does it cost to remove tonsil stones in India?
The cost of removing tonsil stones in India can vary depending on several factors. Generally, the cost of tonsillectomy, which is the surgical removal of the tonsils, starts from around Rs. 55,000 and can go up to Rs. 60,000. However, this is just an estimate, and the actual cost may vary based on a variety of factors such as the medical condition of the patient, the severity of the inflammation, the experience of the surgeon, and the hospital or clinic where the procedure is performed.
What are side-effects of tonsil stones treatments?
If you notice the development of milia on your skin, it is generally not a cause for immediate concern. Nonetheless, there are some circumstances where getting medical help may be a good decision. Here are some situations in which you should consider seeing a healthcare provider;
- If your milia are accompanied by other symptoms, such as redness, swelling, or pain, it may be a sign of an underlying condition that requires medical attention.
- If the milia are located in sensitive areas, such as around the eyes or on the genitals, it is best to have them evaluated by a healthcare provider.
- A more dangerous issue, such skin cancer, could be present if the milia change in size, shape, or color.
- If you have tried over-the-counter medications or home cures without results, it may be time to contact a dermatologist for expert care.
- If the appearance of milia is causing you distress or affecting your confidence, a healthcare provider can help you explore your options for treatment.
Conclusion
Milia are small, benign cysts that typically develop on the skin surface. They often go away on their own over time and are not typically a reason for alarm. However, if you are concerned about the appearance or persistent nature of your milia, there are a variety of treatment options available.
If you have any worries or strange symptoms related to milia, it's crucial to talk to a healthcare professional. Additionally, taking steps to prevent milia through proper skin care practices can help to minimize the risk of their development.
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find ENT Specialist near me
Ask a free question
Get FREE multiple opinions from Doctors