Cornea (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Nov 24, 2022
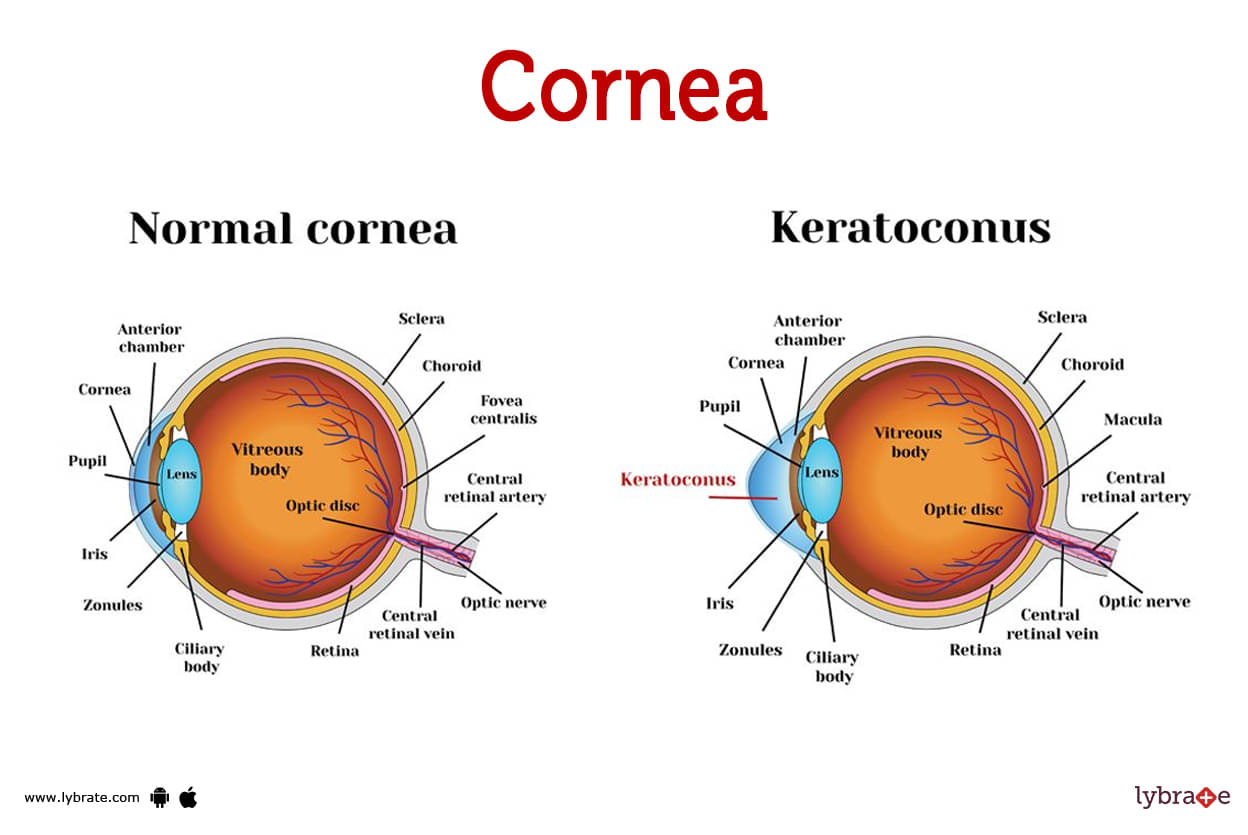
Cornea Image
The cornea is the transparent 'window' at the front of your eye. To some extent, it helps with eyesight. Corneal and visual health can be maintained with proper eyewear, annual eye exams, and care.Each of the five layers that make up the cornea—epithelium, Bowman's membrane, stroma, Descemet's membrane, and endothelium—serves a specific purpose. The transparent cornea protects the eye's anterior segment
Cornea Functions
The cornea is very important for clear vision. The main reason for it is to help the eyes focus. The cornea is just a little bit curved. Light that enters your eye is bent as it travels through the cornea because of how the cornea is shaped.The curve makes it easier for your eye to focus on things that are close or far away.
What are the layers of the cornea?
The cornea has five layers:
- Epithelium: The epithelium makes up the cornea's outermost layer. To protect the eyes from debris and light, it can be worn. Tears supply it with oxygen and nourishment.
- Bowman’s layer: This thin layer serves as a bridge between the stroma (the following layer) and the epithelium (the outermost layer).
- Stroma: Behind the epithelium is the cornea's thickest layer. A combination of water and protein forms its constituent parts. A firm yet malleable stroma The cornea's characteristic dome form is the result of the stroma's outward growth.
- Descemet’s membrane: In between the stroma and the endothelium is this extremely thin layer.
- Endothelium: They form a thin layer of cells between the stroma and the aqueous humour. You're looking at a transparent liquid known as aqueous humour. The stroma can only absorb a certain amount of water, so the endothelium functions as a pump to remove the excess.
Cornea Disorders and Conditions
- Injuries: Minor corneal scrapes can happen, but they usually heal on their own. Scarring of the cornea and subsequent vision problems may result from more severe injuries. It could happen for a number of reasons, some of which are accidental.
- Pink eye: This is also known as conjunctivitis. Eye irritation and allergic conjunctivitis can be brought on by pollen allergies. When an allergy is present, certain symptoms manifest, including redness, itching, and watering of the eyes.
- Keratitis: The term 'keratitis' describes irritation or inflammation of the cornea of the eye. Most cases of keratitis can be traced back to an infection brought on by wearing contact lenses. Redness, itching, and watery eyes are all potential signs of keratitis.
- Dry eye: The cornea becomes inflamed or irritated, a condition known as keratitis. Infections brought on by contact lenses are the leading cause of keratitis. Redness, irritation, and tears are all signs of keratitis.
- Corneal dystrophies: Abnormal chemical deposition in the cornea, the transparent front part of the eye, is a defining feature of this group of extremely rare genetic diseases. Corneal dystrophies are characterised by symptoms such as light sensitivity, cloudy morning vision, and foggy corneas. Night and low-light vision is impaired due to glare and halos.
- keratoconus: Lower and middle corneal layers become thinner in keratoconus. When keratoconus affects the cornea, it can become misshapen and protrude in a conelike fashion. It's possible that this corneal shape causes visual distortions. Astigmatism, sensitivity to light, double and blurred vision, irritated eyes, and difficulty seeing distant objects clearly are all symptoms of keratoconus.
- Fuchs dystrophy: Endothelial cells are unable to function properly due to this disorder. Inability of endothelial cells to function leads to inflammation and a thickening of the cornea. Changes to the cornea can impair vision. Signs include corneal cloudiness, sensitivity to light, and blurred vision upon waking. Night and low-light vision is impaired due to glare and halos.
- Lattice dystrophy: Hereditary lattice corneal dystrophy is marked by amyloid buildup and worsening eyesight. The central cornea is often affected by these deposits, which cause linear, 'lattice-like' opacities. This could cause vision issues. If the cornea's outer layer isn't properly attached and dissolves, it can cause corneal erosion. Symptoms include hazy vision, wet eyes, light sensitivity, and eye pain.
- Map dot fingerprint dystrophy: Patients between the ages of 40 and 70 are more likely to have symptoms of epithelial basement membrane degeneration when it appears in their bodies. It results in corneal creases that resemble continents, dots, or fingerprints. These folds can temporarily impair vision. Corneal erosion can occur when the cornea's outer layer separates from the eye. Morning eye discomfort that improves over the day, hazy vision, wet eyes, and light sensitivity are all symptoms.
- Shingles: Shingles (herpes zoster) When the chickenpox virus reactivates in nerve cells, shingles develops. Shingles can inflame and damage the cornea.
- Ocular herpes: When a herpes virus penetrates the eye, it can produce ulcers on the eyelids or the cornea's outer layer. This is referred to as ocular herpes. Keratitis is a serious eye infection that can result in corneal scarring and loss of vision. If ocular herpes spreads into the cornea or other layers of the eye, it can cause keratitis. Keratitis can be caused by ocular herpes.
- ICE: It occurs when endothelial cells, a kind of corneal cell, move from the cornea into the iris. As they migrate, these cells may obstruct the drainage of ocular fluid, increasing eye pressure. Some of its symptoms include changes in the shape of the iris or pupil, corneal edoema, and the development of glaucoma.
Cornea tests
- Tonometry: Tonometry is the process of measuring the pressure inside your eye. The acronym 'IOP' stands for 'intraocular pressure.'. Tonometry can help your doctor find out if you have glaucoma, a condition that damages your optic nerve.
- Slit Lamp Examination: A slit lamp is a machine that has a very bright light and a special magnifying lens. This machine is used to look closely at the front part of your eye, including the cornea, iris, and lens. If your eye doctor notices anything wrong with your cornea, iris, or lens, he or she will do a thorough examination.
- Fundoscopic Exam: During a fundoscopic exam, the doctor looks at the back of your eye using a special tool called an ophthalmoscope. The ophthalmoscope has a bright light that allows the doctor to see the retina (the back part of the eye), the optic nerve, and blood vessels. This test can help the doctor find problems with these parts of the eye.
How can I prevent injury to my corneas?
Your cornea needs protection, but you can get it. Before performing any of the following, safeguard your eyes with a sturdy pair of eyewear. Use a paintbrush, hammer, and drill to make necessary repairs around the house.Lawn mowing, string trimming, and other forms of yard work can cause grass and dirt to fly in all directions. Sports that use a ball or puck include baseball, tennis, and racquetball. Use materials or equipment.
How can I keep my corneas healthy?
Here are some things you can do to protect your corneas:
- Keep your contact lenses clean by fully disinfecting your contact lenses before each use.
- Regular sanitization is essential. Do what your doctor tells you when it comes to replacing and storing them. It's important to get your corneas checked at regular intervals, so make an appointment with your eye doctor.
- Wear your shades outside. Even while your corneal layer does give some protection from the sun's Ultraviolet radiation, it is nevertheless advisable to wear sunglasses whenever going outdoors.
What should I do if something is stuck in my eye?
- Whenever you feel something foreign lodged in your eye, blink rapidly and forcefully to flush it out. Doing so will cause you to generate tears, which will help wash your eyes out. It is recommended that you flush your eye with saline or sterile water. Eye rubbing can cause scratches on the cornea.
- Do everything you can to get the object out of your eye. As soon as you can, visit an eye doctor or emergency room at a local hospital. Insufficient tear production is the root cause of dry eyes for some people.
- A dry cornea is exceedingly painful and may possibly cause vision loss. Keratitis can be brought on by inflammation or an infection. In most cases of keratitis, the culprit is the wearer's contact lens usage.
Cornea Treatments
- Transplants: The cornea is taken out and replaced by a doctor to treat various instances of this condition. Iridocorneal endothelial syndrome, keratoconus, lattice dystrophy, and a number of other conditions may all benefit from this therapy. With the use of a trephine, an ophthalmologist removes the original cornea. He or she next uses a very tiny stitch to attach the given replacement. The recovery process is accelerated by certain eye drops.
- Cross Linking: To treat keratoconus, an optometrist may utilise corneal crosslinking. UV rays are used in this relatively new treatment. By stabilising corneal tissue, it prevents the illness from progressing. People with severe keratoconus, however, often cannot benefit from the procedure.
- Laser therapy: A computer controlled excimer laser may be used to treat a variety of infections and dystrophies. An ophthalmologist may choose to forego transplantation in certain cases and perform a phototherapeutic keratectomy instead. By destroying unhealthy or abnormal tissue, the laser enables the body to regenerate new tissue. Frequently, patients see speedy healing and eyesight improvements. When just the superficial layer of the cornea has to be repaired, laser treatment performs best.
- Contact Lenses: Ophthalmologists frequently prescribe specialised contact lenses to patients with keratoconus or corneal dystrophies. It's possible that a different kind of lens would work better, but that depends on how severe the issue is. Both flexible and stiff lenses are beneficial in various situations. Patients with early-stage keratoconus may benefit from prescription eyewear.
- Phototherapeutic Keratectomy: In this procedure, a laser beam eliminates diseased tissue, scars, and abnormalities from the cornea's surface. The cornea may be reshaped using PTK in order to enhance eyesight.
Cornea Medicines
- Cyclosporine based medicines for reducing inflammation of Cornea: Ceqa eye drops, which are in the cyclosporine drug class, can be used to treat inflammation. Drugs containing cyclosporine are anti-inflammatory. Also helpful for reducing dry eye symptoms.
- Steroids for reducing inflammation of the cornea: Betamethasone and dexamethasone, two steroid anti-inflammatory drugs, are useful in reducing corneal inflammation.
- Antisclerotic medicines of cornea: It inhibits the enzyme carbonic anhydrase, which belongs to class A. Used for the treatment of a number of corneal conditions, including infection and sclerosis.
- Muscle relaxants for cornea: Its most typical function is to dilate the iris and ciliary body of the eye, allowing for a wider field of vision.
- Antibiotics for infection in Cornea: Antibiotics such as ciprofloxacin and ofloxacin can help with corneal infections.
- Atropine Eye Drops: It belongs to the class of drugs known as antimuscarinics, which help calm the ciliary muscles of the eye.
- Antivirals for treating infection of Cornea: Use of antiviral acyclovir eye ointment has been shown to improve eyesight and decrease corneal infection.
When should I call my healthcare provider about corneal problems?
If your eyes feel scratchy, painful, or look red, you might have a corneal problem. If you experience any of these signs, see a doctor right once.
Table of content
Find Ophthalmologist near me
Ask a free question
Get FREE multiple opinions from Doctors