Corpus Luteum (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Nov 24, 2022
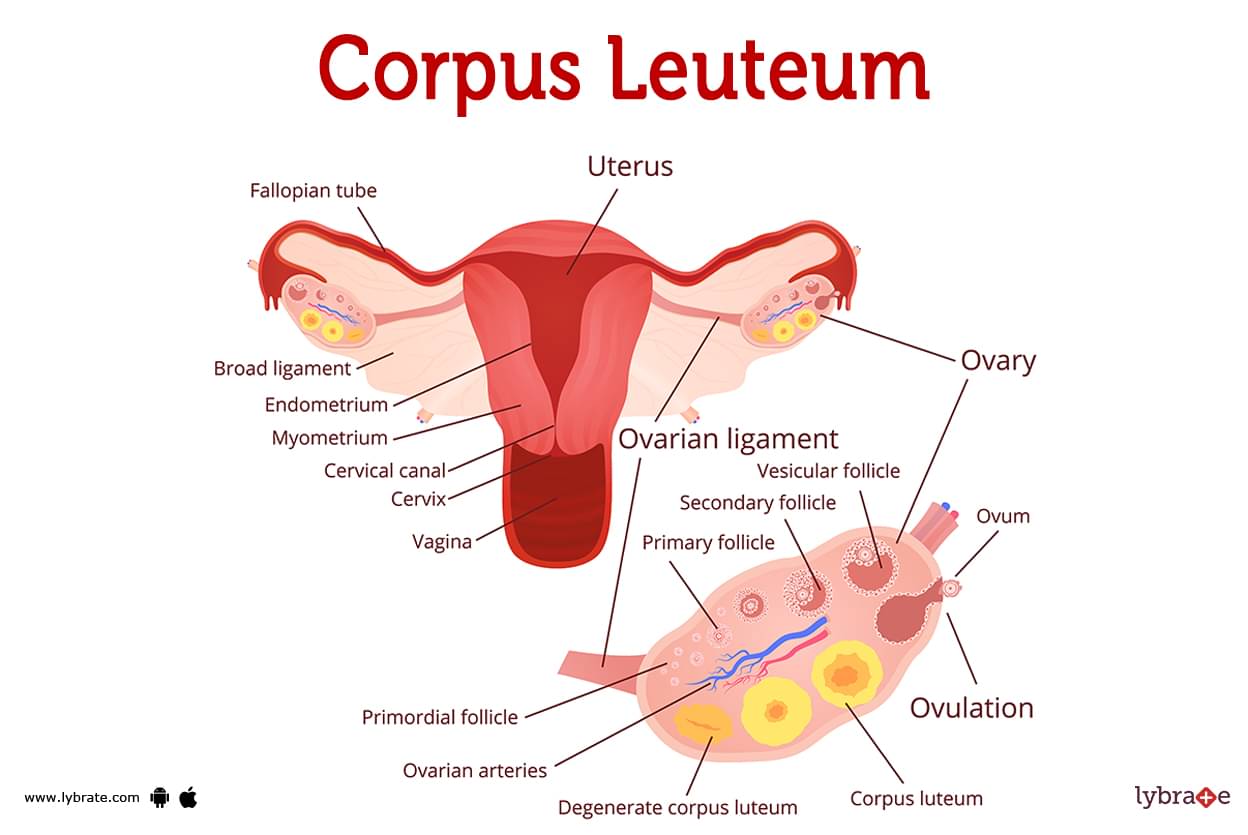
Corpus Luteum Image
The hormone progesterone, which is produced by your corpus luteum, makes your uterus a balanced atmosphere for a growing foetus. Every time you ovulate, a fresh corpus luteum develops, and when you no longer require it to produce progesterone, it disintegrates. Your uterus cannot undergo the changes required for a fertilised egg to develop into a foetus without the corpus luteum.
Every month in women of childbearing age, a cyst known as the corpus luteum develops on the ovary. It is completely normal. This cyst is actually a collection of ovaries-located cells that develops during every menstrual cycle. It manifests as soon as an egg departs your ovary (ovulation). The corpus luteum's function is to maintain the health of your uterus despite being located inside your ovaries.
Corpus Luteum Functions
- When an egg is released from the ovaries, the corpus luteum quickly forms and lasts only long enough to help the uterus sustain a growing embryo. Understanding the stages of your menstrual cycle is helpful in understanding what your corpus luteum does. The corpus luteum plays a crucial role in the third phase (the luteal phase).
- Follicular phase: Small sacs within your ovaries termed follicles are capable of producing eggs (ova or oocytes). A larger, more prominent follicle forms in the initial fourteen days of a female's menstruation. Within it, an egg develops. In contrast, the remaining follicles will gradually shrink and disappear.
- Ovulation Phase: Luteinizing hormones cause the egg to be released from the dominant follicle. The egg may take anywhere from one to two days to emerge from the follicle.
- Luteal Phase: About 14 days pass during the luteal phase. Your corpus luteum begins to develop from the components of the follicle after the egg has exited it. The hormones progesterone and oestrogen are created in your corpus luteum. However, the corpus luteum's primary function is to produce progesterone. The uterus is transformed by progesterone into a favourable environment for a foetus to grow and develop.
Progesterone:
- Makes your uterus larger.
- Creates a more robust endometrium (uterine lining) to better hold a fertilised egg (implantation).
- Keep sufficient oxygen and blood going to your uterus so that an egg can grow into a healthy foetus.
Your corpus luteum has two possible subsequent states:
- The corpus luteum will secrete progesterone for around 12 weeks if the egg is fertilised. In early pregnancy, the corpus luteum is responsible for producing progesterone until about week 12, at which point the placenta begins to produce adequate progesterone for the foetus. In time, the corpus luteum will degrade and shrink.
- After approximately 10 days have passed since the egg has been expelled from the dominant follicle, the corpus luteum of the woman will begin to degrade in the event that the egg does not become fertilised. Your uterus lining won't change without progesterone. Instead, you will experience lining loss when you have your period.
What does the corpus luteum look like?
The corpus luteum sits in the ovary where the dominant follicle used to be. The common conception of a follicle is that it looks like a tunnel, much like a hair follicle; however, the follicles that are located within your ovaries look quite different. Imagine that each follicle is a tiny sac that has the capacity to hold an egg that is developing.
During the process of ovulation, the sac ruptures when the egg is released from the dominant follicle. In the place where the hair follicle used to be, a saffron-colored mass of cells begins to form, which then begins to take the form of a new structure. As it expands, the size of this new structure, which is called your corpus luteum, can be anywhere from slightly less than 2 centimetres to 5 centimetres.
What is the corpus luteum made of?
Two distinct types of cells, called follicular theca cells and follicular granulosa cells, make up the bulk of your corpus luteum. The follicles in the ovaries contain both types of cells. These cells are stimulated to produce progesterone by a hormone known as human chorionic gonadotrophic (HCG).
Corpus Luteum Conditions and Disorders
- Defect in the corpus luteum: This occurs when this organ fails to produce progesterone. Without appropriate levels of this important hormone, the uterine lining will not thicken and maintain a pregnancy.
- Luteal phase defect: When the corpus luteum releases progesterone, the uterus does not respond. This is known as luteal phase deficiency, and it is a prevalent cause of infertility. A corpus luteum cyst is a typical, harmless fluid-filled tumour that develops in the ovaries. It develops on your corpus luteum, a clump of cells that form each month after your ovary produces an egg (ovulation).
- PCOS: causes abnormally high levels of masculine hormones. This hormone imbalance leads their body to skip menstruation and makes it more difficult for them to conceive.
- Endometriosis: It manifests itself as the growth of endometrial-like tissue on the uterine, intestinal, or ovarian walls.
- Perimenopause: It is also referred to as the menopause transitional phase since it occurs prior to menopause.
When the corpus luteum is affected, what symptoms typically present themselves?
If your corpus luteum makes you feel bad, it's probably because of a cyst. Most cysts on the corpus luteum are harmless and don't hurt. As a rule, they decide to left on their own. However, they can be challenging to work with at times. Examples of such indicators include:
- Illness centred in the pelvic region.
- Abdominal satiety.
- Stomachache or urinary discomfort.
- Pain localised to one side of the body.
- Discomfort while making love (dyspareunia).
- Excessive menstrual bleeding in between periods.
- Aching or pain in the breasts or on one side of the body.
A failure of the corpus luteum to produce enough progesterone to allow an egg to embed in the uterine lining may explain why some women have difficulty conceiving or keeping pregnancies going.
Corpus Luteum Tests
- Transvaginal Ultrasound: Your doctor will be able to examine your uterus and ovaries in greater detail with a transvaginal ultrasound. During the process, a delicate wand that emits sound waves will be introduced into your vagina. This will be done in order to complete the procedure. Once it's inside, it sends out pulses of sound waves, which a monitor then displays as a visual. It makes it possible for your healthcare provider to see any lumps, such as a corpus luteum cyst.
- Genes Testing: Your physician may advise you to have a sample of your blood analysed in order to look for gene mutations that are associated with an increased likelihood of developing ovarian cancer. It is helpful for your doctor to know if you have an inherited variation in your DNA before making decisions regarding your treatment strategy.
- Oestrogen Tests: They determine how much oestrogen is present in the body's blood or urine. An at-home test kit may also be used to assess oestrogen in saliva. A tumour of the ovaries may be the cause of elevated levels of estradiol or oestrogen.
- Contrast-Enhanced Computed Tomography CECT: X-rays are used in this scan to detect kidney disease of varying severity.The picture is improved by the intravenous administration of contrast dye, which improves prognosis The use of intravenous contrast dye during this examination may worry renal sufferers.
- MRI: Magnetic resonance imaging of healthy and sick kidneys has promising potential due to the combined value of the anatomical and functional information provided, as well as the distinctive contrast patterns that may be observed non-invasively. Infiltrative kidney disorders can be detected via imaging with several contrasts.
- Ovary Biopsy: A kidney biopsy is a medical procedure in which a small portion of kidney tissue is taken and examined under a microscope. It may be used to detect blockages and structural faults.
Corpus Luteum Treatments
- Laparoscopic ovarian drilling: It is a basic surgical treatment that use heat or a laser to eliminate the tissues that generate male hormones such as testosterone.
- Radiation Therapy: This approach utilizes X-rays to eliminate cancer cells. If alternative treatments have failed to alleviate your problems and you have no intention of becoming pregnant, your healthcare physician may prescribe ovarian removal. Your doctor will employ this laparoscopic technique to remove both the ovary and the fallopian tubes if they are no longer healthy. They may also suggest this procedure to women who have gone through menopause to stop the cancer from coming back.
- Vaginal rings: A vaginal ring is a delicate, flexible, clear plastic ring that you put in your vagina. This is another long-lasting, reversible method of birth control that helps cure PCOS symptoms.
- Cryotherapy to prevent ovarian cancer: At abnormal parts of the ovaries, a very cold probe is put in place. This probe freezes the abnormal cells, killing them, and ignoring the risk of ovarian cancer.
- Preventative laser therapy against ovarian cancer: It involves using a high-powered laser to 'burn' regions of aberrant cells in the ovaries.
- HCG hormone therapy: Chorionic gonadotrophic (HCG) or clomiphene citrate is an option if your doctor determines that your corpus luteum is not producing adequate progesterone. Both hormones initiate processes that stimulate your corpus luteum to produce progesterone, which can be used in place of surgery to eliminate a big or persistent cyst.
Corpus Luteum Medicines
- Antibiotics for an infection in the ovaries: Regular usage of the medicine is recommended by gynaecologists in order to effectively treat vaginitis, trichomoniasis, vaginismus, and other associated disorders. Patients are often given antibiotics that are effective against a wide variety of bacteria, such as ofloxacin, norfloxacin, metronidazole, ceftriaxone, and cefoperazone. In spite of the fact that additional antibiotics such as clindamycin, gentamicin, and doxycycline are routinely utilised in the management of complicated vaginal conditions,
- Antivirals for any ovary-related infection: Even if the exact criteria for these diseases remain unknown, antivirals like ganciclovir, acyclovir, and others are still used to treat conditions like herpes, human papillomavirus, and HIV, all of which are types of sexually transmitted diseases.
- Antifungal medications for fungal infestations: These are available as both dusting powders and topical solutions that can be applied straight to the spot where the problem is occurring. It is also feasible to take drugs like amphotericin, isotretinoin, itraconazole, and luliconazole orally and administer them to a patient through intravenous or parenteral routes on a regular basis, based on the intensity of the infection or the kind of therapy that is required.
Table of content
Find Gynaecologist near me
Ask a free question
Get FREE multiple opinions from Doctors