Epidermis (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Nov 23, 2022
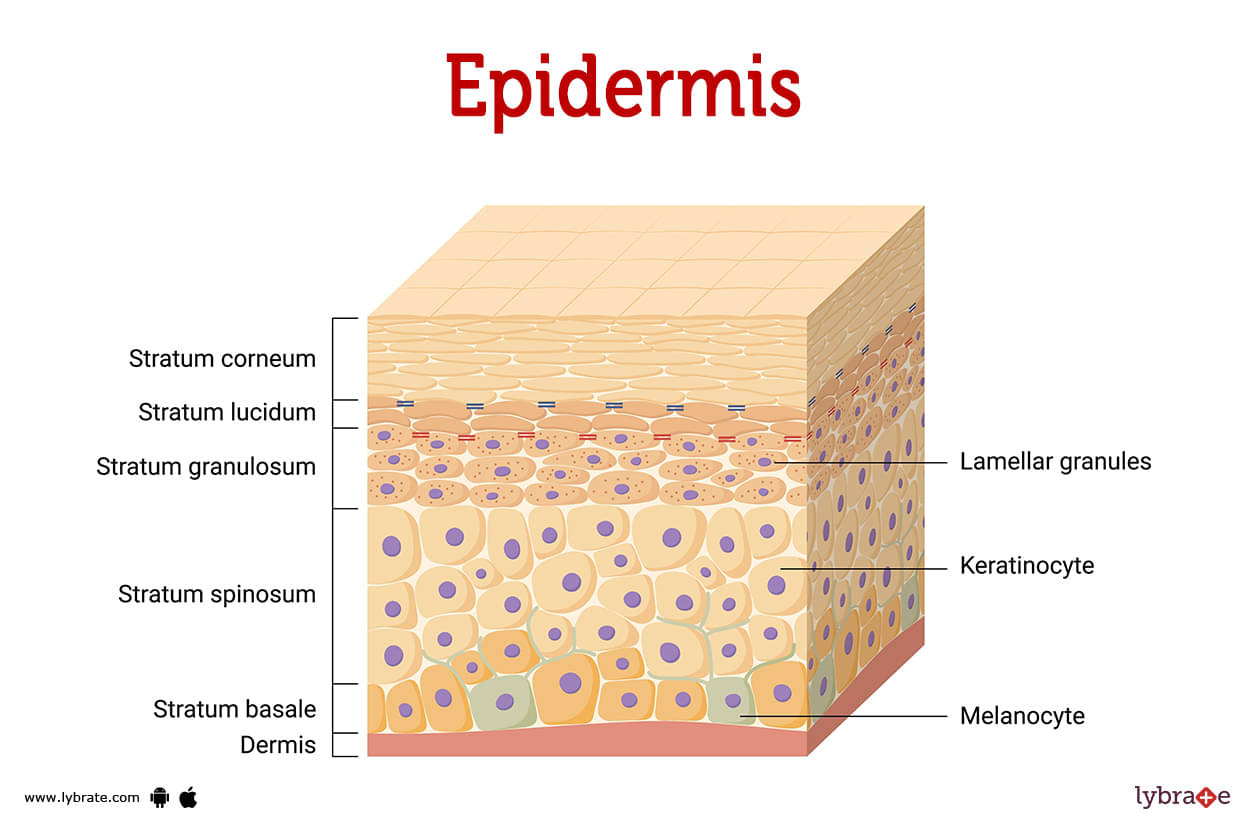
Epidermis Image
The topmost layer of skin on your body is called the epidermis. Gives your skin its colour while protecting it from damage. Keeps you hydrated, regenerates skin cells, and contains melanin, which is essential for dark skin.
Your skin has three main layers, with the epidermis (ep-uh-derm-us) being the outermost layer. Two other layers of skin is underneath the subcutaneous layer. The epidermis is the thinnest layer of your skin, and it protects you from environmental exposure. It consists of five layers altogether.
The term 'epidermis' is derived from the Ancient Greek prefix epi-, meaning 'outer,' and the Ancient Greek word derma, meaning 'skin.' Therefore, the word means 'outer skin.' The order of the epidermis layers is as follows:
- Stratum basale (stratum germinativum): Epidermis' deepest layer.
- Stratum spinosum: It is the epidermal layer between the layers of stratum basale and stratum granulosum.
- Stratum granulosum: It is the layer that exists between the stratum spinosum and stratum lucidum layers.
- Stratum lucidum: It exists between stratum granulosum and stratum corneum.
- Stratum corneum: it is the epidermis's top layer.
What is the difference between epidermis and dermis?
The outermost layers of skin, known as the epidermis and dermis, protect the body from the environment. The thin outer layer of the skin is referred to as dermis. The dermis is the intermediate layer of the skin, located between the epidermis and the hypodermis. The dermis is the thickest layer of skin, in contrast to the epidermis, which is the thinnest. Collagen and elastic fiber are in the dermis and allow it to have structure and strength. The dermis and hypodermis are home to all of your body's connective tissues, nerve endings, sweat glands, oil glands, and hair follicles.
Where is the epidermis located?
When you look at another person or touch them, you are interacting with their epidermis, which is the topmost layer of their skin as well as the layer that is visible to you and can be felt by you.
What colour is the epidermis?
Melanocytes produce skin-coloring melanin. Melanocytes produce two pigment-determining melanins:
- Eumelanin: Your skin, eyes, and hair all have dark colours thanks to this particular type of melanin.
- Pheomelanin: This type of melanin is responsible for the pink or red coloration of your lips, nipples, vagina, and the bulbous structure at the end of the penis (glans), as well as your hair.
How does the epidermis help with other organs?
The stratum corneum and other skin layers provide support for the skeleton, organs, muscles, and tissues.
How big is the epidermis?
The thickness of the epidermis varies throughout your body. Areas of the skin where there is a lot of friction, such as the soles of your hands and feet, have thicker epidermis, compared with areas that have not been subjected to as much friction. These areas can be as thick as 1.5 millimeters, which is about the thickness of two credit cards stacked together.
The epidermis is thinner in other facial regions. For instance, the thickness of the epidermis layer on your eyelids is approximately 0.05 millimeters, which is comparable to a sheet of copy paper.
What are the 3 major cells that make up the epidermis?
The epidermis contains different types of cells, including:
- Keratinocytes: Keratinocytes make keratin, which is the main protein in the epidermis.
- Melanocytes: Your melanocytes are responsible for making your skin's pigment, known as melanin.
- Langerhans cells: Langerhans cells make sure that nothing gets into your skin.
Epidermis Functions
The skin works to promote and protect the body's functional structure, organs, muscles, and tissues. The epidermis serves numerous additional purposes, including:
- Hydration: The stratum corneum, the top layer of the epidermis, holds water and keeps your skin moist and healthy.
- Producing new skin cells: When new skin cells mature, they migrate from the epidermis' basal layer (stratum basale) to the epidermis' upper layers (stratum corneum and stratum granulosum). After about a month, they have reached the epidermis's outermost layer, where dead skin cells are shed and new cells develop at the base.
- Protection: The epidermis serves as a shield that prevents harmful elements, such as ultraviolet (UV) radiation, pathogens (bacteria, viruses, fungi, and parasites), and chemicals, from entering the body and wreaking havoc.
- Skin color: Melanocytes in the epidermis produce melanin, which gives skin color.
What are some common signs or symptoms of conditions that can affect your epidermis?
The following are some common signs or symptoms of conditions that can affect your epidermis:
- Dark spots or growths that change shape or color.
- Dry or cracked skin.
- Peeling or eroding skin.
- Scaly skin.
Epidermis Conditions and Disorders
- Acne: When oil from glands, bacteria, and dead skin cells clog skin follicles, inflammation occurs.
- Alopecia Areata: This disease is aimed at the hair follicles. Most hair loss happens in small, circular patches.
- Atopic Dermatitis: Itchy skin is the result of a skin disorder. Scratching causes itching, redness, swelling, cracking, leaking of a clear fluid, crusting over, and eventual flaking off.
- Epidermolysis Bullosa: The blisters that are caused by this category of illnesses are excruciatingly painful and can manifest themselves in any location on the body. Blisters that are infected can be a nuisance.
- Hidradenitis Suppurativa (HS): Hidradenitis suppurativa, also known as acne inversa, causes pimple-like lumps or boils and skin tunnels.
- Ichthyosis: This disorder causes dry, fish-scale-like skin.
- Pachyonychia Congenita: This unique illness expresses itself in a variety of ways, including enlarged nails and painful calluses on the feet's soles.
- Pemphigus: Blazes are caused by a disorder in which the immune system erroneously destroys healthy cells in the outermost layer of the skin.
- Psoriasis: Psoriasis is a skin disease that causes red, scaly patches that can be itchy, uncomfortable, swollen, or even very hot. Specialists are instructed on the ways psoriasis develops and what causes it.
- Raynaud’s Phenomenon: The sickness disrupts the body's circulation. Your body will temporarily stop delivering sufficient blood to your limbs.
- Rosacea: It's a chronic issue that causes inflammation and acne on the face. The skin may become thickened, and there may be problems with the eyes.
- Scleroderma: Scleroderma not only causes areas of the skin to become rigid and hard, but it also carries the risk of causing damage to the body's blood vessels and internal organs. Investigate the factors that cause and can treat this skin condition.
- Vitiligo: Vitiligo causes skin white spots. Pigment-producing skin cells breakdown causes it. d.
- Actinic prurigo: Sun exposure causes actinic prurigo (AP).
- Argyria: The term 'argyria' describes alterations in skin tone brought on by a buildup of silver in the body.
- Chromhidrosis: A true case of chromhidrosis is an extremely rare disorder that can affect either the apocrine or eccrine sweat glands, resulting in the production of coloured perspiration.
- Harlequin ichthyosis: Having thick, hard patches or plates of skin from birth (known as Harlequin ichthyosis).
- Lamellar ichthyosis: In the first few weeks of birth, people with lamellar ichthyosis lose their waxy outer skin layer, revealing red, scaly skin underneath.
- Necrobiosis lipoidica: This condition, known as necrotizing lipoid necrosis, is an ulcerative rash that typically affects the lower legs (sores).
- Epidermal Nevus Syndromes: Nevi are benign skin growths that form when there is an overabundance of cells in the outermost layer of the skin's epidermis (epidermis ). Oftentimes, infants and young children will notice the appearance of harmless epidermal growths known as nevi.
- Blau syndrome: Particularly susceptible to the inflammatory effects of Blau syndrome are the skin, joints, and eyes.
- Familial cold urticaria: The uncommon inflammatory condition known as familial cold urticaria is passed down through generations of a family and is brought on by being exposed to cold temperatures. The condition is characterised by recurrent bouts of rash, fever, joint pain, and other symptoms that point to inflammation throughout the body.
- Hyper-IgD syndrome: Hyperimmunoglobulin D syndrome, a rare autosomal-recessive genetic condition, causes recurrent fever, lymphadenopathy, stomach pain, and high blood polyclonal IgD levels.
- Cold sore: Cold sores are tiny, uncomfortable blisters caused by the herpes simplex virus. Herpes simplex labialis, also known as fever blisters, is a typical viral skin infection.
- Hives: Hives, also known as urticaria, are red, itchy bumps that develop on the skin. Red, pink, or flesh-colored; may occasionally sting or hurt. Most people who experience hives do so as a result of an allergic reaction.
- Actinic keratosis: Actinic keratosis is a rough, scaly area on the skin caused by excessive sun exposure. It is commonly found on the facial regions, lips, ears, forearms, scalp, neck, and backs of the hands.
- Carbuncle: Carbuncles are a grouping of boils (sore, pus-filled lumps) that have merged to form a larger infected region beneath the skin.
- Latex allergy: Rubber gloves, condoms, and other medical devices are all made of natural rubber latex, which can cause a latex allergy if the user's immune system reacts abnormally to one or more of the latex proteins.
- Basal cell carcinoma: Basal cell carcinoma is a legitimate form of skin cancer. The cells that give rise to basal cell carcinoma are the skin's basal cells, which continually replenish the skin's surface as old cells die.
- Squamous cell carcinoma: This prevalent form of skin cancer affects the squamous cells that line the dermis and epidermis.
- Melanoma: The cells (melanocytes) that produce melanin, the pigment that gives your skin its color, are also targeted by melanoma, the deadliest form of skin cancer. Melanoma can occasionally affect internal organs such as the nose and throat. Additionally, melanoma can develop in the eyes.
Epidermis Tests
- Biopsy: The word 'biopsy' refers to the process of taking a small piece of skin to look at under a microscope.
- Culture: A sample of skin can be grown in a lab to look for bacteria, fungi, or viruses.
- Skin patch test: A skin patch test, in which tiny amounts of a chemical are put on the skin, can be used to find out if someone has an allergy.
- Black light examination or Wood light test: Examining your skin's pigmentation with the help of ultraviolet (UV) light (a 'black light' examination or 'Wood light test') (a 'black light' examination or 'Wood light test').
- Diascopy: In the diagnostic procedure known as diascopy, a patch of skin is placed under a microscope slide, and any colour change that occurs is observed.
- Dermoscopy: When conducting a dermoscopy exam, a physician will use a hand-held device known as a dermatoscope to investigate the patient's skin in order to arrive at a diagnosis.
- Tzanck test: examining the fluid from the blisters for any indications of herpes simplex or herpes zoster.
Epidermis Treatments
- Laser therapy: Laser resurfacing of the skin can improve the appearance of fine wrinkles and scars, even out skin tone (pigmentation), tighten sagging skin, and remove benign and malignant tumours.
- Skin graft: A skin graft occurs when healthy skin is transplanted from one place of the body to another where there is damage or missing tissue. When there is a substantial quantity of tissue loss (as in the case of cancer or burns), when the skin is damaged after a bone fracture (open fractures), or when there is a large incision, they are used.
Epidermis Medicines
- Antivirals for Epidermis infections: The body's natural defences against virus infection are supported by antiviral medications. The drugs can shorten the duration of a viral illness and lessen the severity of symptoms. Acyclovir, valaciclovir, famciclovir, penciclovir, cidofovir, foscarnet, and immune response modulator are a few examples.
- Antiprotozoal for Epidermis infections: Antiprotozoal medications are used to treat parasitic infections brought on by the single-celled organisms known as protozoa. We may single out Nitazoxanide Albendazole Artemether-Lumefantrine Dihydroartemisinin-Piperaquine as one of the many examples accessible.
- Chemotherapeutic Medicines for Epidermis cancer: Cisplatin, doxorubicin, mitomycin, and 5-fluorouracil are some drugs that may be prescribed for cancer treatment. Adults with basal cell carcinoma may be treated with the vismodegib capsule under a doctor's supervision.
- Steroids for Epidermis cancer: Inflammation produced by immune-related cancers such as basal cell carcinoma is treated with glucocorticoids. Furthermore, glucocorticoids have the capacity to suppress the immunological system. Corticosteroids include dexamethasone, prednisolone, methylprednisolone, and hydrocortisone, to name a few.
- IV steroids for Epidermis infections: Systemic steroids that are commonly used in the treatment of Epidermis infections include prednisone, prednisolone, methylprednisolone, dexamethasone, and hydrocortisone.
- NSAIDS for Epidermis infections: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen, and a variety of other medications are the most effective treatment for mild to moderate pain.
- Liposomal Medicines for Epidermis infections: In select cases, amphotericin B liposomal is injected to treat fungal infections. Among these illnesses are cryptococcal meningitis, a fungal infection of the spinal cord and brain, and visceral leishmaniasis, a parasitic disease that often affects the spleen, liver, and bone marrow.
Simple lifestyle changes/tips to keep your skin healthy.
- Establish a skin care routine and adhere to your healthcare provider's advice to maintain healthy skin.
- Use a gentle soap in the shower or bath, and pat your skin dry instead of rubbing it. Applying a moisturiser right after drying your skin will help keep the moisture in. Cream or ointment should be reapplied two or three times a day.
- Use warm water for baths or showers, not hot water.
- Drink at least eight glasses of water each day. A hydrated skin is a healthy skin.
- Consume antioxidant-rich foods such as fruits, vegetables, legumes, fish high in omega-3 fatty acids and nuts for optimal health.
- Avoid sudden changes in temperature and humidity.
- Reduce the amount of irritants and allergens that you are exposed to.
- Make sure that the sunscreen you use has an SPF of at least 30.
- It is important to refrain from scratching or touching injured skin.
Table of content
Find Dermatologist near me
Ask a free question
Get FREE multiple opinions from Doctors