Excretory system (Human Anatomy): Image, Function, Diseases, and Treatments
Last Updated: Mar 17, 2023
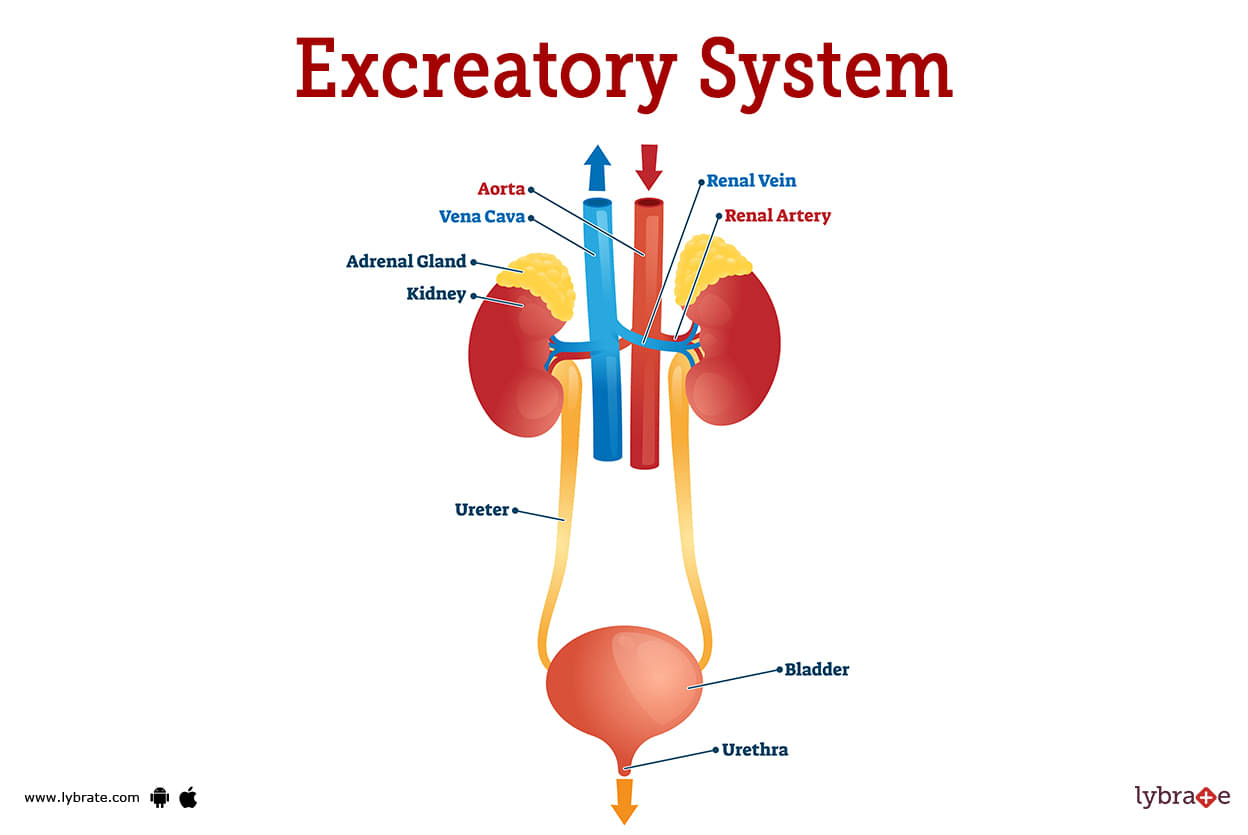
Excretory System Image
The kidneys, ureters, bladder, and urethra make up what we call the excretory system. This mechanism cleanses your blood of impurities and extra fluid. Urine is the product of this waste. Infections of the urinary system and the bladder are the most prevalent genitourinary problems (UTIs).
The genitourinary system consists of the ureters, bladder, and urethra, in addition to the kidneys. The blood is filtered, getting rid of toxins and extra fluid. As a result, urine is produced. Urinary tract infections and bladder infections are the most frequent genitourinary conditions (UTIs).
Excretory System Functions
Kidneys, ureters, bladder, and urethra make up the excretory system. Your blood is filtered to eliminate all the junk and extra fluid. Urine is produced from this waste. Bacterial infections of the urinary tract and the bladder are the most prevalent urinary problems (UTIs). Identifying and removing harmful substances while keeping beneficial ones. The process of collecting one's urine for later elimination.
Excretory System Conditions
- Acute Renal Injury: When the kidneys abruptly stop working correctly, it's called acute kidney injury (AKI), although it's more frequently known as acute renal dysfunction (ARF).
- Chronic Renal Failure: Renal failure or damage can develop unexpectedly and only last a few days in an episode known as acute kidney injury (AKI), also known as acute renal dysfunction (ARF).
- Acute Renal Dysfunction (ARF): An episode of renal failure or damage that develops unexpectedly and lasts for a few hours to a few days is called acute kidney injury (AKI), also known as acute renal dysfunction (ARF).
- Pyelonephritis: Pyelonephritis is an infection that has migrated from the kidneys to the bladder. Symptoms of this condition include burning micturition, nausea, vomiting, and abdominal pain.
- Glomerulonephritis: Pyelonephritis is when an infection has moved from the kidneys to the bladder. In this case, you'll have scorching micturition, frequent nausea and vomiting, and abdominal pain.
- Nephrolithiasis, Or Kidney Stones: Different types of calculi are found in the urinary tract. The two conditions are distinct; kidney stones (nephrolithiasis) and urethral stones (ureterolithiasis) are found together.
- Ureteric Calculi: They almost always begin in the kidneys, even if they end up in the ureter. Renal calculi often contain calcium as one of their main components.
- Renal Colic Pain: Renal colic pain is caused by dilatation, stretching, and spasm of the ureter because of acute ureteral obstruction.
- Nephrotic Syndrome: Acute ureteral obstruction induces dilatation, strain, and spasm, all of which contribute significantly to renal colic pain.
- Kidney Cysts: Renal colic is characterized by severe discomfort because of acute ureteral obstruction, which results in dilatation, stretching, and spasm.
- Polycystic Kidney Disease: The kidneys grow and lose function over time due to polycystic kidney disease (PKD), a genetic condition characterized by the formation of clusters of cysts.
- Acute Renal Failure: Acute renal failure is characterized by the sudden inability of the kidneys to filter waste products from the bloodstream. The loss of your kidneys to filter your blood can lead to an unhealthy accumulation of waste materials and an imbalance in your blood's chemical makeup.
- Chronic Kidney Failure: Patients with chronic kidney disease, also known as chronic kidney failure, see a gradual reduction in renal function over time. Because of the accumulation of fluid, electrolytes, and wastes, chronic kidney disease can be life-threatening.
- End-Stage Renal Disease (ESRD): Chronic kidney disease, the gradual decline in kidney function, can lead to a terminal condition known as end-stage kidney disease or renal failure. If you have end-stage renal disease, your kidneys cannot filter blood effectively enough to meet your body's demands.
- Papillary Necrosis: Renal papillary necrosis is a disease of the kidneys that results in the death of all or part of the renal papillae. The kidney papillae are the openings via which urine enters the ureters and the collecting ducts.
- Diabetic Nephropathy: Diabetic Nephropathy (DN), also known as diabetic kidney disease, is characterized by a decline in glomerular filtration rate (GFR) and significant levels of urine albumin excretion in people who have diabetes. As a frequent consequence of both type 1 and type 2 diabetes, diabetic Nephropathy affects the kidneys.
- Hypertensive Nephropathy: It is a medical condition that depicts the damage done to the kidneys due to long-term hypertension.
- Nephrosclerosis: It's important to distinguish this form of secondary HTN from renovascular hypertension, which has a different etiology and mode of action.
- Pyonephrosis: When the ureters get blocked, a suppurative infection known as pyonephrosis develops. This often leads to suppurative damage of the renal parenchyma and a reduction in renal function. Patients often have symptoms, yet up to 15% of those diagnosed may persist in lacking signs. A life-threatening infection in pyonephrosis can develop into urosepsis if surgery is delayed.
- Hydronephrosis: Hydronephrosis refers to kidney enlargement due to a urinary pee backup. An obstruction prevents urine from generally passing from the kidney to the bladder, leading to this condition. You can have hydronephrosis in one or even both kidneys.
- Cancer Of The Kidney: Cancer of the kidney is a phrase used to describe the development of malignant metaplasia in the kidney. One kidney sits behind each set of abdominal organs on either side of your spine.
- Interstitial Nephritis: When the spaces between the renal tubules enlarge, interstitial nephritis sets up (inflamed). There may be a decrease in renal function as a result of this.
- Minimal Change Disease: Nephrotic syndrome is another possible complication of this illness. Protein in the urine, low blood protein levels, high cholesterol, high triglyceride levels, and swelling indicate nephrotic syndrome.
- Perinephric Abscess: Symptoms include repeated pain, fever, and discomfort, and the condition is characterized by an accumulation of pus around the kidney that has progressed by cortical extension and hematogenous channels.
- Genitourinary Tuberculosis: Hematogenous spread of TB from the lungs causes a secondary infection of the kidneys. The kidney is a critical organ in this process, and the prostate is also impacted.
- Renal Agenesis: One or both kidneys do not develop normally due to a congenital abnormality known as renal agenesis. Unilateral agenesis refers to the condition in which only one kidney is affected, whereas bilateral agenesis describes a situation in which both kidneys are missing.
- Emphysematous Pyelonephritis (EPN): The gas accumulation in the tissues is caused by a severe infection of the renal parenchyma. People with diabetes mellitus, especially women, are at increased risk for EPN. Similar to acute pyelonephritis, this condition presents with a set of uncomfortable symptoms.
- Hyperuricemia: Uric acid crystals in the glomeruli cause renal parenchyma inflammation, ultimately resulting in renal failure.
- Hematuria: Hematuria is a medical condition defined by detecting blood in the urine. Possible that it will have no harmful effects. It may result from anything as benign as a urinary tract infection or as severe as bladder cancer.
- Urinary retention: It occurs when a blockage or restricted bladder muscles prevent urine from escaping. If the bladder retains more pee than usual, it may swell.
- Cystocele: When pelvic muscles weaken after birth. This causes cystoceles when the bladder presses on the vagina. They can't urinate.
- Bladder tamponade: When pelvic muscles weaken after birth. The bladder pushes on the vagina, generating cystoceles. They have problems urinating.
- Nocturia: Children who wet the bed once or twice a week for at least three months are deemed to have bed-wetting. It may be a behavioral issue caused by the child's anxiousness or lack of motivation, or it may be caused by improperly functioning bladder muscles.
- Dysuria: Refers to pain or discomfort while urinating. Infection, irritation, or all three can cause urinary bladder, urethra, and external genital inflammation.
- Urinary tract infections: Painful urination refers to discomfort when discharging pee. Urinary bladder, urethra, and external genital inflammation can be caused by infection, irritation, or all three.
- Interstitial cystitis: Refers to pain or discomfort during urinating. Infection, irritation, or all three can cause urinary bladder, urethra, or external genital inflammation.
- Urinary incontinence: Lack of bladder control causes this widespread, painful condition. Depending on how bad it is, you may leak pee when you cough or sneeze or need the restroom so urgently you can't get there.
- Bladder trauma: Direct contact on an enlarged bladder, high-energy traumas that disrupt the pelvic floor, and penetrating and iatrogenic injuries are all potential causes of this highly uncommon injury.
- Neurogenic bladder: It occurs when the link between the nervous system and bladder function is broken, usually due to an accident or sickness. Because of this, there is no known cure, but the symptoms can be treated.
- Hunter's ulcer: Bladder ulcers develop on the bladder wall and, like other ulcers, can bleed, leak, and come in different sizes.
- Fowler's syndrome: It's a factor in young women developing urinary retention. Painful urinary retention is unusual in young women but can occur. The urethral sphincter is where the trouble begins (the muscle that keeps you continent).
- Bladder diverticula: When the bladder's urothelium and mucosa protrude through the muscularis propria, they create a thin-walled structure that drains poorly during micturition. Bladder diverticula are hereditary or environmental.
Excretory System Test
- Urinalysis: A urine study can reveal diabetes, bladder stones, chronic kidney disease, and bladder infections.
- USG urinary bladder: This test uses sound waves to create a picture of the urine bladder. It can identify abnormalities in the size and form of the urinary bladder as well as blockages such as tumors and stones.
- CT scan: In this test, a picture of the bladder is created by ultrasound. It can reveal blockages like tumors or stones, as well as abnormalities in the size and form of the urinary bladder.
- Contrast Enhanced Computed Tomography CECT: This scan uses X-rays to identify urinary bladder diseases; intravenous contrast dye offers a more accurate diagnosis. Patients with urinary bladder difficulties may be worried about this test, which uses intravenous contrast dye.
- MAG 3 Study: Mercaptoacetylglycine is used to diagnose renal perfusion. It's used to diagnose renal perfusion.
- MRI: MRI of healthy and sick urinary bladders provides tremendous promise due to the anatomical and functional information supplied and the distinctive contrast patterns that may be observed non-invasively. Multiple contrasts demonstrate infiltrative bladder disorders.
- Blood Urea Nitrogen (BUN): When ingesting protein, your body creates urea nitrogen. BUN levels should be 7-20. Renal impairment raises blood BUN levels.
- Ureteroscopy: A ureteroscope is introduced into the urethra, bladder, ureter, and stone site to treat urinary bladder stones. The operation takes one to three hours under general anesthesia.
- Urinary Bladder Biopsy: In ureteroscopy, a tiny telescope called a ureteroscope is inserted into the urethra and bladder, up the ureter, and into the area where the stone is lodged. While under general anesthesia, the procedure usually takes one to three hours to complete.
- Pressure Flow Study (Whittaker Test): This treatment requires percutaneous bladder puncture and pelvic contrast. Take pelvic pressure. Increased intra-pelvic pressure suggests pelvic ureteric junction obstruction.
Excretory System Treatment
- Extra hydraulic lithotripsy: These procedures use electrohydraulic pressure to break up kidney stones. This minimally invasive technique is the top standard for treating nephrolithiasis.
- Suprapubic cystolithotomy: This surgery involves making an incision in the lower abdomen and removing the stone from the bladder part whole rather than damaging the bladder wall.
- Cystoscopy: Bladder stone removal surgery is making an incision in the lower abdomen and removing the stones one at a time instead of using a fragmentation technique.
- Exploratory laparotomy: This method involves making an incision in the lower abdomen and removing bladder stones by hand rather than breaking them up.
- Cystolithopaxy: Bladder stones are mineral deposits that occur inside the bladder and are usually treated with surgery. It is a popular method used by adults to exchange bowel movements stored in their bladders. It's a cutting-edge example of minimally invasive surgery.
- Urine cytology: Bladder stones are painful mineral deposits that can only be removed surgically. Sexual action often involves exchanging adult urinary bladder feces. It's minimally invasive.
- Ureteroscopy: Urinary tract infections, cysts, Abscesses, and tumors of the bladder and urethra can all be diagnosed with this process by inserting a small scope into the bladder and returning it.
- Laparoscopic stone surgery: through little incisions made with a laparoscope instead of a large one. Unlike other, more intrusive methods, this one requires only a little incision to remove a significant number of stones.
- Anderson Hynes dismembered pyeloplasty: In this newer traditional way, the ureter is moved to cross the lower pole vessels. This is done to improve the performance of the pile of plastic.
Excretory System Medicines
- Steroids for Reducing inflammation of the Excretory system: Anti-inflammatory medications prevent polymorphonuclear leukocytes (PMNs) from migrating to cellular and tissue injury areas, reducing inflammation. Methylprednisolone is an example of a helpful corticosteroid.
- Analgesics for pain in the Excretory system: The pain-reducing mode of action of these medications includes preventing polymorphonuclear leukocytes (PMNs) from migrating to areas of cellular and tissue injury, hence reducing inflammation. Methylprednisolone is a common and valuable corticosteroid.
- Antibiotics for infection in the Excretory system: Drugs with anti-bacterial effects work by preventing polymorphonuclear leukocytes from migrating to areas where cells and tissues have been damaged, decreasing inflammation. The corticosteroid methylprednisolone is among the most significant.
- Diuretics: In the Excretory system: for reducing inflammation, these medicines limit PMN migration to areas of cellular and tissue injury. Methylprednisolone is a corticosteroid.
Frequently Asked Questions (FAQs)
What are the 5 diseases of the excretory system?
What happens when the excretory system goes wrong?
How do you take care of your excretory system?
How can you prevent diseases of the excretory system?
What are the common causes of excretory system problems?
What helps the excretory system?
Table of content
Find Urologist near me
Ask a free question
Get FREE multiple opinions from Doctors