Prolapse Surgery: Purpose, Procedure, Benefits and Side Effects
Last Updated: Jun 30, 2023
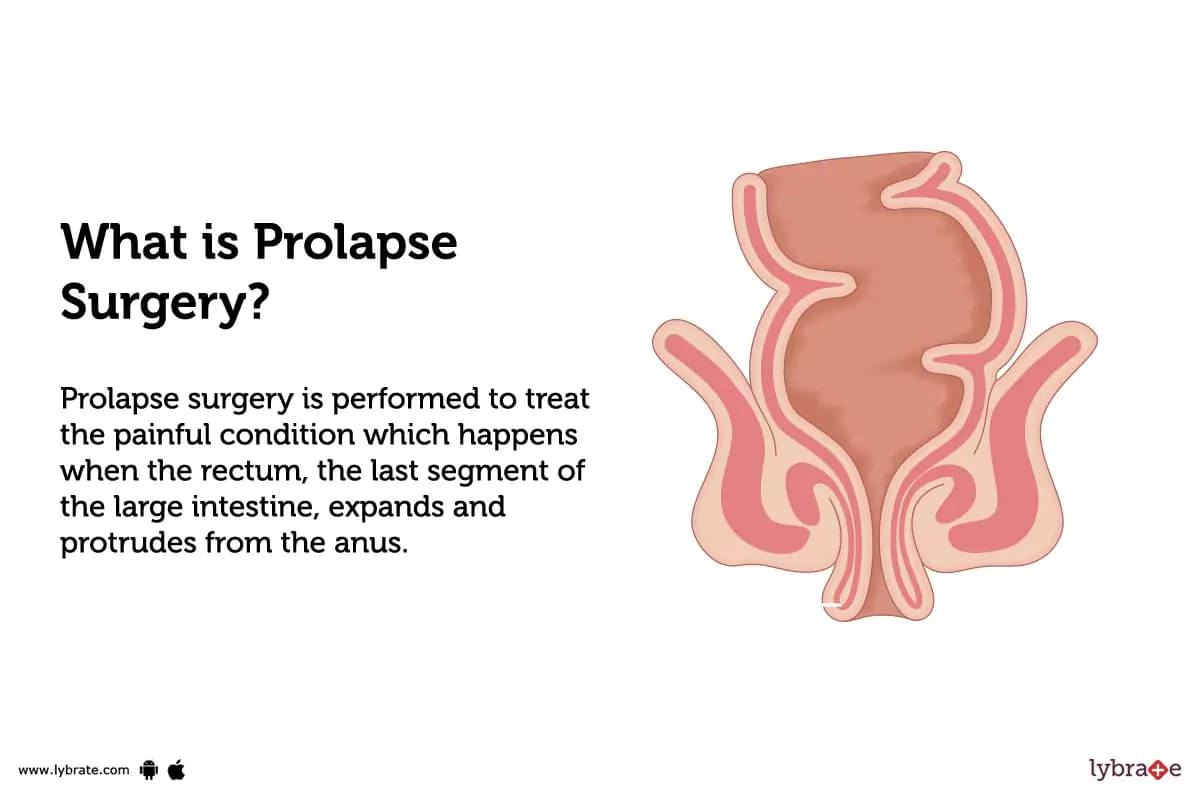
What is Prolapse Surgery?
Prolapse surgery is performed to treat the painful condition which happens when the rectum, the last segment of the large intestine, expands and protrudes from the anus. People who experience persistent rectal prolapse symptoms like stool leakage, fecal incontinence, or obstructed bowel movements as well as the pain and suffering are usually treated with surgery to manage their symptoms.
The majority of rectal prolapse surgeries are performed under general anesthesia. However, spinal anesthesia or epidural anesthesia may also be administered for elderly or very frail patients.
To treat rectal prolapse surgically, there are basic surgical procedures which are specific to your condition and the one which is best for you will be determined by your surgeon.
Types of Prolapse Surgery
There are various types of surgery that can be used to restore the prolapsed rectum. The two main types of prolapse surgery are:
Obliterative surgery
In this procedure, the prolapse is adjusted by closing some portions of the vaginal canal which helps to reduce viscera back to the pelvis.
Reconstructive surgery
Reconstructive surgery helps to bring back normal anatomy and redresses the prolapsed vagina.
Summary- The types of prolapse surgery are: obliterative surgery and reconstructive surgery.
Benefits of Prolapse Surgery:
As rectal prolapse can be pretty embarrassing and may cause several health problems in long run, surgery can elevate the quality of life of the patient with the following benefits;
- Relief from constipation
- Relief from pain during intercourse
- Relief from bleeding from recto vagina fistula
- Relief from the rectal bulge
- Other pelvic organs may also be treated and corrected during the surgery
- Reduces the chance of a prolapse
- Reduces pressure on the vaginal walls
- Reduces bowel problems
- Reduces bladder issues
- Provides better quality of life
- Provides support to the prolapsed organs
- Relieves pain
Summary- Prolapse surgery helps to correct the prolapsed organs, relieves pain, reduces bowel and bladder problems and provides better quality of life.
Why is Prolapse Surgery done?
When your problem is not getting solved through medicines and therapeutic measures and your prolapse has entered into the final stage of its maturity then doctors usually recommend surgery. Even though surgery is not always required, it is necessary for the effective treatment of rectal prolapse. Prolapse prevention, defecation function restoration, and prevention of constipation or incontinence are the three main objectives of the treatment. Prolapse surgery is highly required to treat complications of rectal prolapse that include;
- Intestinal leakage: Your anal muscles may become more difficult to hold in gas and excrement as they continue to stretch. Most of the patients who have rectal prolapse report this problem.Constipation. You can have trouble passing your stool if your rectus muscles are bundled up or if you have poor muscle coordination. Some people experience incontinence and constipation in cycles.
- Stomach ulcers: Rectal ulcers and uncomfortable, bleedable sores can be brought on by friction and exposure of the mucous lining of your rectum. Anemia could result from uncontrolled bleeding.
- Strangulation of the rectum: Due to incarceration, the risk of 'strangulation' also increases in which the blood supply is cut off. This can cause the rectum's tissues to degenerate. Long-term untreated conditions including faecal incontinence and nerve damage are possible outcomes.
Summary- Prolapse surgery is done for the treatment of stomach ulcers, intestinal leakages, strangulation of the rectum and incarceration.
What are the risks of Prolapse Surgery?
Possible complications of rectal prolapse surgery include:
- Allergic reaction to the anesthetic
- Hemorrhage
- Bowel obstruction
- Onset of west or new constipation
- Sexual dysfunction
- Infection
- Injury to nearby nerves or blood vessels
- Fistula — an abnormal connection between the rectum and vagina filled with abcess
- Damage to other pelvic organs, such as the bladder or rectum
- Death (necrosis) of the rectal wall
- Recurrence of the rectal prolapse.
Risks can vary from patient to patient depending on their age, prolapse grade and surgical technique used to treat the condition.
Summary- The risks of prolapse surgery are: hemorrhage, infection, injury, bowel obstruction and fistula.
How do I prepare for Prolapse Surgery?
Your doctor could want you to do the following to get ready for surgery for rectal prolapse:
- Use specialty soap to clean: You will be instructed to use antiseptic soap in the shower prior to surgery in order to reduce the risk of infection from bacteria on your skin.
- Empty stomach: You will be asked to be on an empty stomach eight to ten hours prior to the treatment.
- Stop using specific drugs: Your operation may require you to stop using a particular medicine.
Following rectal prolapse surgery, you'll stay in the hospital for one or more days. To ensure that you'll be as comfortable as possible during your stay in the hospital, consider bringing:
- Items for personal care, such a toothbrush, a hairbrush, or shaving materials
- Comfier attire, such as a robe and pajamas.
Summary - You should stop taking any medications, or food items and wear loose clothes before going for the surgery.
How Prolapse Surgery is done?
Rectal prolapse surgery is the only option to treat the condition in adults as prolapse in younger kids mends on its own while elderly and frail are very seldomly treated with surgery due to the complications it can have on their health. The procedure of prolapse surgery also depends on the severity of the condition, that includes:
- Internal prolapse: The rectum has prolapsed internally, but not far enough to pass through the anus, hence also known as an incomplete prolapse
- Mucosal prolapse: Mucosal prolapse is when the rectum's internal lining protrudes through the anus
- External prolapse: The entire thickness of the rectum comes out of the anus. This is also known as complete or full-thickness prolapse
The first option for individuals in fairly good health and less severe prolapse is typically a rectopexy, which involves fixing your rectum through your abdomen. But not everyone is a good candidate for abdominal surgery. Rectal surgery is another choice in certain circumstances. To know how the prolapse surgery is done, read the step-by-step description provided below;
Summary - Prolapse surgery can be done in two ways: rectopexy and abdominal surgery.
Before the procedure
- The patient is asked to be on an empty stomach eight to ten hours prior to the treatment.
- The patient is typically admitted a day before the procedure and relaxed on all medical parameters.
- Depending on what surgical method the doctor determines, either general or local anesthetic may be administered. In the spinal block your lower half will be numbed, and in general anesthesia you will be put to sleep.
- Surgery for rectal prolapse can be performed through the abdomen (rectopexy) or the area around the anus (perineum). Which method your surgeon chooses will depend on a variety of variables, including the extent of your prolapse, your age, any coexisting medical conditions, your surgeon's experience, personal preferences, and the equipment at hand. Overall, there is no preferred method. Hence, discuss your alternatives with your surgeon.
During the procedure
- Repair of rectal prolapse (Abdomen): Using an abdominal incision, the surgeon pushes the rectum back into position. He or she fastens the rectum to the pelvic back wall using stitches or a mesh sling. Sometimes, such as when there has been a long history of constipation, the surgeon will cut off a section of the colon.
- Laparoscopic surgery for rectal prolapse (Abdomen): This surgery, which is also carried out through the belly, making multiple smaller incisions. To correct the rectal prolapse, the surgeon makes small abdominal incisions and inserts specialized surgical instruments and a tiny camera.
- Laparoscopic surgery (Abdomen) with robots: Similar to a laparoscopic procedure, a surgical robot is used in this kind of surgery.
- Repair of rectal prolapse via Perineal Rectosigmoidectomy (Anus): The surgeon pulls the rectum through the anus, removes a piece of the large intestine and stitches or staples the rectum and colon parts of the intestine together during the most often used version of this treatment, Altemeier procedure. This type of repair is often only appropriate for people who cannot have an open or laparoscopic procedure.
- Whereas another perineal rectosigmoidectomy method is employed for short prolapses, which are more frequently treated with the Delorme procedure, another technique for correcting a rectal prolapse through the perineum. To shorten the rectum, the muscle layer is folded and the lining of the rectum is removed.
- You might have both repairs done in one surgery if you have rectal prolapse along with other diseases like vaginal prolapse or pelvic organ prolapse.
After the procedure
- Hospital staff will keep track of and record your blood pressure, temperature, pulse, and breathing
- You will be given medicine to treat your pain. Tell your nurse if you need more pain medication
- You'll stay in the hospital for a short period of time (4-6 days) to heal and regain your bowel function.
- An intravenous fluid line will be implanted in your arm to replenish lost body fluids
- You'll start out by consuming clear liquids before moving on to solid foods. Depending on the surgery you have, you may only need to stay in the hospital for one night
- The patient will have an abdominal or vaginal gauze bandage dressing as there will be some vaginal bleeding. The pad will be removed later that day or the day after surgery
- A catheter will be inserted in some patients to empty their urine until they can empty their bladder on their own. The catheter is taken out before the patient is released
- For 48 hours, the patient is asked not to shower. Swimming after that is likewise not advised
- In the weeks following surgery, your doctor may advise drinking lots of fluids, using stool softeners, and eating a fiber-rich diet to prevent constipation and excessive straining, which can result in a recurrence of the rectal prolapseMost patients can resume their regular activities 4 to 6 weeks after surgery
- Relearning how to use the pelvic floor muscles may be necessary for some persons during physical therapy
- You must make follow-up appointments with your doctor.
How much does Prolapse Surgery cost?
The price of Prolapse surgery can range from Rs. 3,50,000 to Rs. 6,00,000.
What to do after Prolapse Surgery?
Some selfcare can help you with the recovery of prolapse surgery, which include;
- Stool softeners used: Patients will be instructed to consume stool softeners after surgery to lessen excessive bowel movement strain. This promotes healing and guards against further damage to the repaired rectum. In the early stages of recovery, using stool softeners will also be crucial for pain control.
- Changing diet to promote healing: Patients will be instructed to modify their diets in addition to utilizing stool softeners to avoid constipation and straining when passing their bowels. Typically, patients would begin their diets with clear liquids before introducing soft meals and then solid foods over the course of a few weeks. Diets high in fiber will be most beneficial throughout this healing time. Pay close attention to any dietary suggestions that your surgeon makes.
- Drink lots of water: Patients should consume plenty of fluids and maintain a healthy level of hydration while they recuperate in order to keep stools soft and prevent challenging bowel movements. Stick to water and stay away from alcohol, soft drinks, and sugary drinks.
- Avoid strenuous activity and heavy lifting: Patients should refrain from heavy lifting and all other forms of intense activities for a few weeks to reduce the risk of complications and re-injury. This entails cardiovascular exercise, squatting, and waist bending. You can get guidance on when you can resume these activities from your surgeon.
- Taking a off from office: Patients must take time off from work due to the nature of the prolapse repair operation. Please be aware that while you recuperate, you may need to reduce some of your responsibilities when you return to work or ask your employer for reasonable accommodations.
- Follow-up visits to the doctor: Throughout the healing process, your surgeon will schedule numerous follow-up appointments. This will enable you to track your recovery and ensure that you do not experience any health issues as you recover. Attend each of these appointments, and get in touch with your surgeon if you have any urgent concerns.
Summary- You should take a nutritious diet, avoid exhaustive activities and take proper care of the incision areas after the surgery.
What to eat after Prolapse Surgery?
- Grains, bread, and cereals (without added fiber)
- White bread, white rice
- Vegetables
- Whole grains
- Juices made from strained vegetables without pulp
- Vegetables without seeds, stalks, or skins
- Desserts and fruits
- Soups, casseroles, and cream sauces
- Pudding or custard
- Protein-rich foods such as meat
- Nut-free peanut butter
- Eggs
- Butter, milk, margarine, and oils
- Honey, sugar, and syrup
Summary- You should take a diet rich in protein and fibre after the prolapse surgery.
Is Prolapse Surgery safe?
Yes, prolapse surgery is safe for healthy people and provides quality of life to the patients. However, people with other health conditions or weakness are either treated with perineal rectal surgery or they are suggested to wear supportive inner clothing to avoid rectal prolapse.
Is Prolapse Surgery painful?
As rectal prolapse surgery is performed under local or general anesthesia, the patients are hardly in senses to feel any pain or discomfort during the procedure. Although, after the surgery they can experience some pain, depending upon the type of technique employed, for which they are given pain-killers from the attending nurse staff.
How long does it take to recover from Prolapse Surgery?
After a prolapse surgery, recovery takes place between 4 to 6 weeks. However, recovery periods following a vaginal or laparoscopic surgery are frequently shorter and may take about 1 to 2 weeks.
Summary- After prolapse surgery, recovery could take one or two months.
What are the side effects of Prolapse Surgery?
Common side-effects that may occur after prolapse repair surgery include:
In order to reduce post-operative discomfort, your surgeon will suggest painkillers and over-the-counter pain drugs. Additionally, suggestions for sitting and sleeping arrangements will be given in order to lessen pain while you are recovering.
Summary- The side effects of prolapse surgery are: bleeding, swelling, bruising and soreness.
Prolapse Surgery Aftercare
- Some aftercare tips for prolapse surgery are:
- Rest as much as you can
- Increase your intake of fibre.
- Drink 6 to 8 glasses of water every day
- Take a ten-minute sit bath three times a day
- Exercise frequently
- Maintain a healthy weight
- Don’t strain on the toilet.
- Avoid using enemas or inserting anything into the rectum
- Avoid Strenuous activities
- Walking is recommended for exercise
- Attend your surgeon's follow-up appointments timely
Summary- Post-treatment guidelines for prolapse surgery are: take a healthy diet, maintain a healthy weight, do exercises and avoid any strenuous activity.
Conclusion
Rectal prolapse typically happens as a result of a slow, progressive loss of muscle. Even though it is not a medical emergency, it can be upsetting when it does. While the condition is unavoidable, self-care can always help. You may maintain the greatest condition for your pelvic organs by exercising your pelvic floor muscles and paying attention to your bowel health. If prolapse does occur, it can be treated surgically.
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find Urologist near me
Ask a free question
Get FREE multiple opinions from Doctors