Prolapse: Symptoms, Causes, Treatment, and Cost
Last Updated: Feb 25, 2023
What is prolapse?
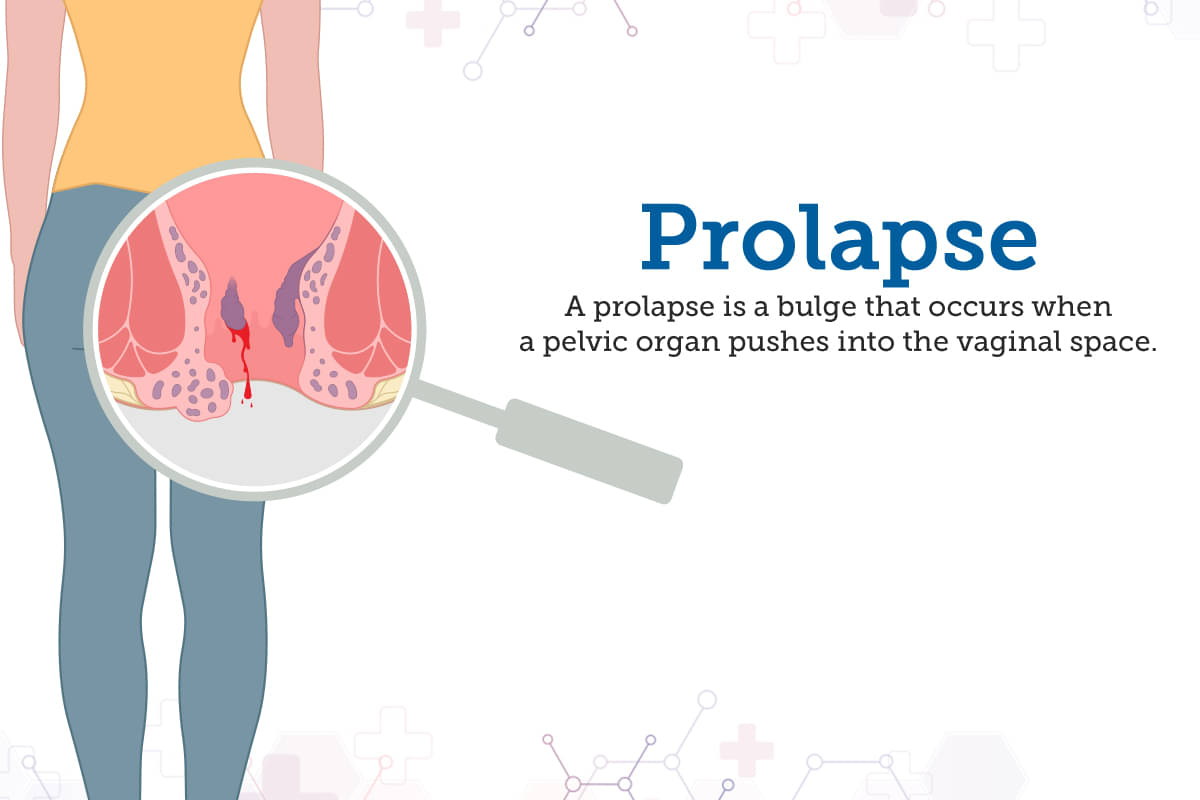
When one or more pelvic organs slide down from their normal position, the condition is referred to as prolapse. After misplacing these organs bulge into the vagina. These organs may include the bowel, bladder, uterus, or top of the vagina.
However, prolapse does not possess life-threatening issues but it leads to recurring pain and discomfort.
Summary- Prolapse occurs when one or more pelvic parts misplace at their original sites.
How serious is a prolapse?
A prolapse is often considered a serious disorder that must be addressed on time. It does not threaten life but can disrupt a normal lifestyle. Its treatment must not be delayed otherwise it will worsen the symptoms.
Summary- Prolapse is often considered a serious problem as it exerts some adverse effects on the body.
What does a prolapsed uterus look like in pictures?
Uterine prolapse occurs in almost 50% of women, especially between the ages of 50 and 79. Prolapse happens when the pelvic muscles and tissue become weak, causing the uterus to drop into the vagina. Sometimes, the prolapsed uterus can be visible through the vaginal opening.
Summary- Uterine prolapse is the most common type of prolapse experienced by most women.
Types of prolapse
Prolapse is differentiated under the following categories.
Vaginal prolapse
Sometimes, the structural support of the vagina weakens and drops from the normal position into the lower vaginal canal or even projects out of that. This situation is marked as vaginal prolapse.
Pelvic organ prolapse
Pelvic organ prolapse is experienced when pelvic organs like the womb, bladders, or bowel, bulge into the vagina. Multiple prolapsed pelvic organs may occur in a patient at once.
Uterine prolapse
Whenever the uterus slides down into the vaginal canal and in some cases even protrudes outside it. This situation is named Uterine prolapse.
Rectal prolapse
Rectal prolapse takes place when the rectum separates out from the vagina because the front part of the rectum pushes through the thin tissue which is the rectovaginal septum.
Cord prolapse
When the umbilical cord enters the vagina before the infant through an open cervix, it is known as cord prolapse in women. It may occur before or during childbirth, but it needs to be addressed right away. However, it is a rare case.
Disc prolapse
Disc prolapse occurs due to the injured fibres of the intervertebral disc. This situation is often commonly known as a herniated disc. This type of prolapse is mostly observed in middle-aged and young adults.
What are the symptoms of prolapse?
While pain and discomfort is the most common symptom of a prolapse, some prolapses can also be seen, and are visible to the naked eye. Let us explore some symptoms of prolapses.
Vaginal prolapse
It is not necessary that you may feel any symptom of a vaginal prolapse. However, some symptoms that you may experience are:
- A heaviness or fullness in the pelvic area. The feeling could get worse during standing, coughing, or lifting
- A visible bulge in the vagina
- Lower back pain
- Urinary incontinence or inability to control urine
- Bladder infections
- Difficulty in inserting a tampon
- Problem during sexual intercourse
- Difficulty in defecating
Pelvic organ prolapse
Some symptoms of pelvic organ prolapse are:
- Heavy feeling around the genitals or the lower abdomen
- Discomfort inside the vagina
- Feeling of sitting on a small ball or feeling of something in the vagina
- Numbness during secual intercourse
- Difficulty in urinating - or feeling that the bladder is not emptying properly, needing to urinate more often, or urinating a little during sneezing, coughing, or exercising
Uterine prolapse
The symptoms of uterine prolapse are the same as the symptoms of the pelvic organ prolapse. In addition to the usual symptoms, a feeling of constipation is also a symptom.
Rectal prolapse
The first symptom of rectal prolapse will be experienced during bowel movement. Some other symptoms are:
- A feeling of a bulge outside the anus
- Visually seeing a red mass outside the anal opening
- Pain the rectum or the anus
- Rectal bleeding
- Leakage of faeces, blood, and/or mucus from the anus
Cord prolapse
One of the first symptoms of an umbilical cord prolapse is a sudden decline in the foetal heart rate that does not get resolved immediately.
Disc prolapse
The main symptoms of a herniated disc prolapse are:
- Loss of bladder or bowel control
- Numbness in and around the genital area
- Impotency in men
- Numbness or tingling sensation in the legs or arms
- Pain in the buttocks or the shoulder blades
- Dull ache running down the arms
Summary- Different kinds of people possess different symptoms.
What causes prolapse?
Some of the causes of prolapses in women are:
- Childbirth: A normal or a vaginal childbirth increases the risk of a prolapse, more than a Caesarian section (C-Section). In a C-Section, the baby is birthed through an opening in the wall of the abdomen. Also, if the baby is bigger, it increases the risk of prolapse.
- Surgery: Any surgery such as removal of the uterus (hysterectomy) or radiation therapy can cause a prolapse in women.
- Menopause: When a woman goes through menopause, the ovaries stop producing estrogen. This hormone keeps the pelvic muscles strong. As and when the body reduces the amount of estrogen produced, the pelvic muscles prolapse.
- Ageing: Older women are at a greater risk of developing prolapse. As you get older, the muscles and tissues weaken.
- Extreme physical activity: Strain from physical activity can weaken the pelvic muscles. Lifting heavy objects is also a cause.
- Genetics: A pelvic support system can also be weaker than usual. This is often due to hereditary factors.
Some other causes of prolapse are:
- Difficulty in defecating
- Constipation
- Being overweight
Suffering from chronic cough - common in smokers and people with asthma
Summary- Some of the common causes of prolapse include hereditary factors, age, childbirth, some underlying disorders, etc.
Who is more prone to suffer from Rectal prolapse?
Rectal prolapse occurs in both men and women. Some of the common causes of this disease are:
- History of diarrhoea or constipation
- Difficulty in defecating
- Straining during defecation
- Weakening ligaments and muscles caused by old age
- Any past injury to the hip or anal area
- Spinal cord disease or any other neurological problem
- Nerve damage
- Injury to the spine
Summary- People undergone some injury or accident or suffer from any underlying disorders are prone to prolapse.
How can you prevent rectal prolapse?
Do's
To reduce the probability of prolapse, follow these tips.
- Kegel exercises: Kegel exercises are the best and most effortless way to strengthen the pelvic muscles. These exercises are important, especially after childbirth.
- Eat healthy: Eat healthy and a high fibre diet including fruits, beans, whole grains, and vegetables. Stay hydrated to prevent constipation.
- Control the cough: Avoid coughing too much, and get treated for bronchitis. Also, avoid smoking.
Don'ts
- There are certain activities that must be avoided, especially as they can put you at risk of prolapse.
- Healthy body weight: Maintain a healthy body weight, and avoid gaining weight, as this will tend to weaken the tissues and the muscles.
- Avoid heavy lifting: If you need to lift something heavy, lift with your legs instead of the back of the waist.
Summary- One may try to prevent rectal prolapse by applying the above-stated simple pathways.
Prolapse: Diagnosis and Tests
In order to diagnose a prolapse, you will need to visit your healthcare professional. The medical provider might perform a physical examination and discuss your symptoms or other conditions. You might also be asked about any past pregnancies or family history of prolapse.
During the pelvic exam, the doctor will ask you to bear down, in the motion of bowel movement. This will help the doctor assess how far the pelvic organ has fallen into the vagina.
You might also be asked to tighten the pelvic muscles, as though you are trying to control the urge to urinate. This will inform the doctor about the strength of the pelvic muscle. Visit an expert doctor at Pristyn Care, and get the correct diagnosis of your prolapse.
Summary- Prolapse is diagnosed with the help of several diagnostic tests along with a detailed physical examination.
What tests are done for prolapse?
In order to diagnose a pelvic organ prolapse, the doctor performs some diagnostic tests to check the conditions and severity of the prolapse. Some of these tests are:
- Ultrasound: If the symptoms are indicative or organs shifting out of place, an ultrasound exam may be prescribed. The ultrasound exam used sound waves to create images of the pelvis, helping the doctor determine the severity of the prolapse. You are not required to prepare for an ultrasound beforehand.
- MRI scan: A MRI scan may be prescribed, in which magnetic waves are used to create images of the pelvis, showing the extent of the prolapse. The MRI allows the doctor to get a clear view of the organs, helping the doctor decide if surgery is needed.
- Cystoscopy: A cystoscopy is an examination which allows the doctor to view the inside of the bladder. An endoscope, a thin tube with a light and camera on one end, is inserted through the urethra, all the way to the bladder. The procedure is performed under local anaesthesia, and analyses bladder pain and the urge to urinate.
- Urodynamics: If the prolapse causes bowel or urinary incontinence, urodynamic tests might be performed to determine the cause. Urodynamic studies the urination speed and volume, bladder pressure, how much urine the bladder can hold, and the amount of urine left after it is expelled. A cystourethrogram is an X-ray test, which shows pictures of the bladder and urethra before and during urination.
Summary- The diagnostic test for prolapse include cystoscopy, lab tests, urodynamics, MRI, and ultrasound.
What are possible complications of prolapse?
A pelvic organ prolapse is rarely life threatening, but can affect the quality of life, causing some problems. Some possible complications of prolapse are:
- Urinary incontinence or bladder control problems
- A issue with the urethra, making it harder to urinate
- Bowel incontinence, with liquid or solid stool coming out
- Painful sexual intercouse
- Urinary tract infections
- Kidney damage
Summary- Some possible complications of prolapse include infections, damage to the kidney, painful copulation, etc.
Home remedies for prolapse
There are some home remedies that can be done in order to provide relief from prolapse. Prolapses must be treated, as they can cause pain and discomfort in the future. Adopt a good lifestyle and healthy eating habits to reduce the risk of developing prolapse.
Kegel exercises: Kegel exercises help strengthen the vaginal muscles and tissues, and are especially recommended after childbirth.
- Avoid smoking as this causes chronic cough.
- Maintaining a healthy body weight and diet.
- Using proper lifting techniques.
- Avoid lifting heavy weights alone.
- Keep your back straight and lift with the knees and hips.
- Keep the feet apart, having a wider stance.
- Hold the object closer to your body, keeping the arms bent and core tight.
These home remedies can only prevent or alleviate rectal prolapse. Doctors recommend surgery to fix this problem and reclaim a normal life.
Summary- There are numerous home remedies available outside for prolapse treatment. However, they cannot cure the disorder completely.
What to eat in a prolapse?
A diet with high fibre and stool softening food should be incorporated in the diet, helping prevent constipation and bowel straining. The food items that should be eaten are:
- Fruits like apples, pears, apricots, peaches, prunes, grapes, and oranges
- Vegetables like squash, carrots, sweet potatoes, kale, green beans, and spinach
- Wholegrain cereals and breads
- Kidney beans and other pulses
- About 1.5 litres of water per day
Summary- Healthy foods must be included in everyday meals to combat prolapse.
What not to eat in a prolapse?
Highly fattening food that increases weight, causes diarrhoea or constipation, high fat food, and food items causing bloating should be avoided in case you have a prolapse.
- Avoid food containing high sugar like chocolates, ice creams, sweets, and soft drinks
- Avoid high FODMAP food like honey, figs, chickpeas, dairy products
- Avoid low fibre food like processed food, meat, cheese, and fast food
Summary- Foods containing high amounts of sugar and salt must be excluded from the diet during prolapse treatment.
Prolapse treatment
Which doctor to consult for prolapse?
You can first visit your general physician, who will recommend a qualified obstetrician-gynaecologist to you. These are specialised doctors who will either guide you on the non-surgical approach to treating the prolapse, or even perform prolapse surgery. There are some specialised urogynaecologists who you can refer to as well.
Visit Pristyn Care and get a consultation with the expert panel of specialised doctors and general physicians.
Summary- One must consult a specialist obstetrician-gynaecologist for complete prolapse treatment.
Prolapse treatment without surgery
There are two non-surgical options to treat the prolapse. These two options are:
- Pelvic Floor Muscle Training (PFMT): This method is effective if the prolapse is mild, but is not very successful in curing advanced or even moderate prolapse. To do this exercise, tighten your pelvic muscle, hold it tightly for a few seconds, and then release. Do this 10 times, and you can do these exercises anywhere.
- Vaginal pessary: A unique device, a vaginal pessary is round in shape, and is placed in the vagina. The pessary supports the uterus, bladder, and rectum, keeping them in shape. Fitting a vaginal pessary usually takes very little time, and can be a short or even a long term treatment plan. The pessary has to be removed and cleaned regularly, and removed before having sex.
The non-surgical methods generally subside the symptoms and also leave a big possibility of recurrence of the condition. Surgery, on the other hand, is something which fixes the problem for good.
Summary- The non-surgical treatment for prolapse usually involves vaginal pessary and pelvic floor muscle training.
Which are the best medicines for prolapse?
There are certain medications which work very well in curing prolapse, especially the ones caused in women.
Estrogen is a good treatment option, as prolapse is often caused due to a lack of this hormone. Most women who suffer from prolapse are in menopause, causing lower estrogen levels. A lack of estrogen weakens the pelvic floor muscles, causing vaginal dryness, among other issues.
However, systemic estrogen should only be taken with care, and under supervision of the doctor. Contact your healthcare provider for better information. You can also visit an expert doctor at Pristyn Care.
Summary- Doctors advise some medications for prolapse treatment often including estrogen.
What are the surgical treatments for prolapse?
For more serious and advanced cases of prolapse, you can opt for a surgical treatment. Surgeries have been proven to be most effective in treating different kinds of prolapse.
- Vaginal vault suspension: This procedure of treating prolapse is done through making an incision. This prolapse involves the small bowel, the rectum, and the bladder. This surgery can either be performed through the vagina or the abdomen.If the surgeon opts for the vaginal approach, the vagina is attached to the ligaments inside the pelvis by making an incision. The abdominal approach is laparoscopic in nature, and the surgeon attaches the vagina to the tailbone. The surgeon might use some synthetic mesh to support the vaginal tissues.
- Posterior prolapse: A posterior prolapse surgery is used to treat prolapses via the rectum. In this method, the connective tissue between the rectum and the vagina are secured, thereby reducing the size of the bulge. During surgery, the excessive tissue will also be removed.
- Anterior prolapse: An anterior prolapse surgery is used to treat prolapse via the bladder. Also called a cystocele, the bladder is pushed back up, and the connective tissue between the bladder and the vagina is secured. Any excessive tissue is also removed. In case you suffer from urinary incontinence, the doctor will suggest a sling or a bladder neck suspension, used to secure the urethra.
- Uterine prolapse: This surgery is like a hysterectomy, where the uterus is removed. This is an effective cure to treat uterine prolapse.
- Colpocleisis: This surgery to treat prolapse stitches the vagina shut. The biggest advantage of this procedure is that the chances of recurrence of the prolapse is low. However, once the procedure is performed, you can no longer have penetrative sex, as the vagina has been stitched shut. This procedure is most popular among older women who suffer from prolapse.
Summary- These above-stated options are the surgical treatment for prolapse. These are often advised by doctors to treat specific prolapse situations.
What is the procedure of prolapse surgery?
Different kinds of prolapse surgery have different procedures. The procedure has been discussed in brief. Discuss with your doctor to know more details about the procedure.
Summary- Treatment of prolapse involves different surgical procedures.
How long does it take to recover from prolapse?
The recovery period after a prolapse surgery depends on the nature of the surgery. In case of open surgeries, the recovery might take 4-6 weeks. In case of keyhole surgeries, only 1-2 weeks is required for complete recovery.
After a pelvic organ prolapse surgery, you will need to stay in the hospital for a few days, till the bladder is functioning properly.
In rare cases, a catheter might be required. You will need to visit the hospital again to have the catheter removed.
Summary- The recovery phase of prolapse is variable for different patients. It may range from 1-2 months.
What is the price of prolapse treatments in India?
When surgical correction is done to treat the vagina for prolapse, it provides relief from prolapse symptoms. In India, the cost of a prolapsed uterus surgery will range anywhere from Rs. 80,000 to Rs. 2,00,000.
Summary- The treatment procedure for prolapse costs about 1-2 lacs.
Are the results of the treatment permanent?
Most of the time, treatment and surgery to treat prolapses are quite effective. However, in some cases, a prolapse can recur. This usually happens if you have had a serious prolapse, got the prolapse when you were younger, or are obese.
Summary- The treatment result is usually permanent. However, some cases are exceptions.
What are the post treatment guidelines?
Follow some tips that will make the post treatment period better, and keep the prolapse at bay. Be sure to listen to your body during the healing process.
- Take any OTC medication if you feel any discomfort or pain
- Rest when required, and lie down every few hours
- Shower regularly, but avoid taking a bath. Gently pat the incision dry with a soft cloth to avoid agitating it
- Use sanitary pads to stop any bleeding that you might experience. Also, the bleeding stops some time in 4 weeks.
- Wear loose and airy clothes that don’t put pressure on the abdomen or the waist.
- The doctor might advise the use of vaginal estrogen tablets or creams.
- If you experience bloating, massage the stomach in a clockwise motion to help ease the pain.
- Reduce the intake of tea, coffee, and alcohol as they are diuretics.
- Avoid lifting heavy objects.
- Avoid smoker’s cough, as it strains the pelvic floor muscles.
- Avoid gaining weight as it puts pressure on the pelvic region.
- Refrain from sexual intercourse till you have healed completely. Also, when you have sex, be prepared to experience a little discomfort.
Summary- Doctors often provide some post-treatment guidelines to smoothen the recovery phase.
What are side effects of prolapse treatments?
There are a few risks or side effects that are associated with prolapse surgery. However, if the surgeon is an expert, the chances of these side effects happening are significantly lower. These side effects are:n
- Allergic reaction to anaesthesia
- Damage to the bladder or bowel
- Discomfort during sexual intercouse, but this will improve over time.
- Vaginal bleeding
- Vaginal discharge
- High temperature
- Acute pain in the stomach
- Burning sensation during urinating
Summary- Prolapse surgery possesses some side effects like- vaginal bleeding, fever, recurring pain, nausea, etc.
Prolapse - Outlook/prognosis
Prolapse is a common problem that most women go through. If you follow the doctor’s advice and suggestions with care, recovery is fast and easy, and you will soon go back to your daily life and routine with no problem.
Be prepared to understand that every body is different, and that recovery and symptoms of each person is different.
Follow the advice of your doctor or healthcare professional, and don’t worry about your prolapse. Visit a doctor at Prisytn Care to get the best care available.
Summary- Prolapse can be tackled with proper treatment and care. We must be vigilant about its treatment procedures.
Frequently Asked Questions (FAQs)
Can you get pregnant with a prolapsed uterus?
What does a prolapse feel like inside?
What should I avoid if I have mitral valve prolapse?
Can a menstrual cup cause a prolapse?
Can you have intercourse with a prolapsed uterus?
Does uterine prolapse cause bleeding?
Can hypopressives make prolapse worse?
Can you push a prolapse back into place?
What happens if you leave a prolapsed uterus untreated?
References
- Prolapse - NHS [Internet]. nhs.uk 2022 [Cited 06 October 2022]. Available from:
- Prolapse - Webmd [Internet]. webmd.com 2022 [Cited 06 October 2022]. Available from:
- Prolapse - Healthline [Internet]. healthline.com 2022 [Cited 06 October 2022]. Available from:
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find Gynaecologist near me
Ask a free question
Get FREE multiple opinions from Doctors