Pubic Symphysis (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Nov 28, 2022
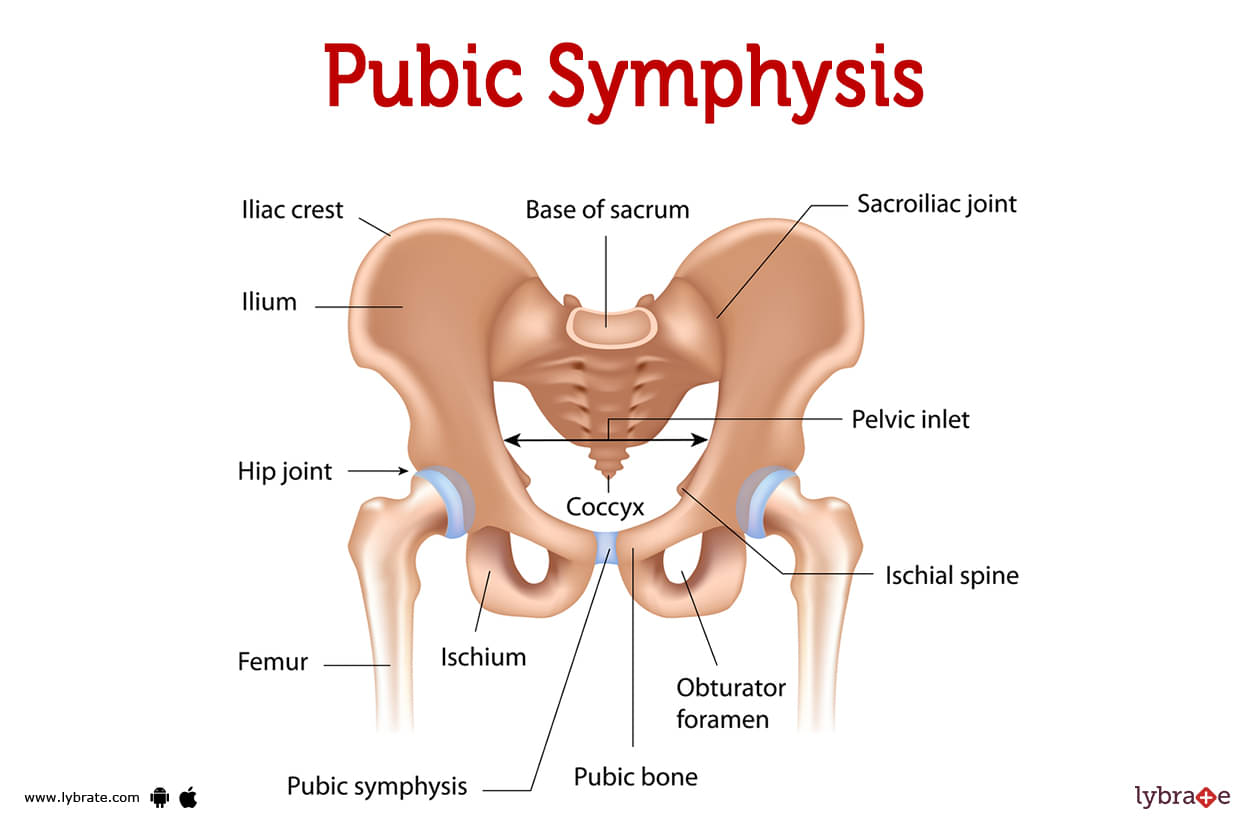
Pubic Symphysis Image
Between your left and right pelvic bones, there is a joint called the pubic symphysis. It enables your upper body's weight to be partially absorbed by your pelvis before it transfers to your lower body. In order to get ready for vaginal delivery, it also aids in separating your pelvic bones.Your pelvic bones on the left and right are connected by your pubic symphysis. Your pubic symphysis is not very mobile, compared to joints like your elbow and knee. Holding the left and right pelvic bones in place is one of its main responsibilities. Nevertheless, it does make minor motions that assist your pelvis in distributing the weight of your upper body. When you are pregnant, these joint movements become considerably more pronounced. During pregnancy, the joint becomes more flexible, allowing your pelvic bones to spread for delivery of the child.
Pubic Symphysis Functions
Your left and right pelvic bones are joined by the pubic symphysis to create a single pelvis that is both strong enough to support your body and flexible enough to expand during birthing. Each pelvic bone is connected by a joint, which creates nearly mirror representations of them.
Weight is distributed from your upper body down your legs and feet through the joint action of your pelvic bones. Your pubic symphysis joint has a range of motion of up to 2 millimetres and a degree of rotation. This motion helps your pelvis absorb trauma while you run or stroll.
This joint is highly important if you are expecting. It becomes more flexible, enabling the baby to pass through the delivery canal and your pelvic bones to widen.
Where is the pubic symphysis?
- Your pubic symphysis joint is located at the base of your pelvis, where your left and right pelvic bones meet. The front of the joint is approximately 3 to 5 millimetres larger than the back. It is located in front of the bladder and above the clitoris and penis.
- Some tendons of the abdominal and thigh muscles attach to ligaments in the public symphysis.
- Tendons originating from your thigh muscles (gracilis).
- Tendons from your oblique muscles (obliquus externus).
- Tendons originating from abdominal muscles (rectus abdominis).
What is the pubic symphysis made of?
Your pubic symphysis joint is made up of two types of cartilage and four ligaments, which make the linkage between your pelvic bones strong but not rigid. The pubic symphysis lets you move a lot more than the joints that link up the bones in your head, but less than joints such as your elbow.
- Fibrocartilage disk: Type I collagen is the main component of the dense fibre mesh that makes up fibrocartilage. Strong skeletal structures rely on type I collagen, which is also found in skin, tendons, and connective tissues like joints. Fibrocartilage fibres consolidate in the pubic symphysis joint to form a thick, fibrous disc. The fibrocartilage disc is held in place by the attachment of ligaments and tendons.
- Hyaline cartilage coating: Type II collagen dominates in hyaline cartilage. The majority of cartilage is composed of type II collagen. The end of the bones of your pelvis are cushioned with hyaline cartilage. In your pelvis, the fibrocartilage disc is located between the left and right hyaline cartilage.
- Ligament connectors: In order to prevent the fibrocartilage disc from slipping or moving more than it should, four distinct ligaments attach to it: the superior pubic ligament, the inferior pubic ligament, the anterior pubic ligament, and the posterior pubic ligament.
Pubic Symphysis Conditions and Disorders
- Tailbone/Coccyx Fracture: The tailbone's location near the very end of the spine makes it susceptible to fracture. If a baby exits the birth canal at an incorrect angle or exits too soon, its tailbone might get sprained or even fractured.
- Fibromyalgia: The symptoms of fibromyalgia, a form of rheumatic condition, include pain and stiffness and musculoskeletal system as well as rigidity and regional discomfort in certain body regions. These symptoms are what define fibromyalgia because of its autoimmune disorder-related origin.
- Pelvic Inflammatory Disease: PID, or chronic pelvic inflammatory disease, is a condition that may result from a protracted infection that is frequently sexually transmitted and can cause pelvic organ-related scarring. Chronic pelvic inflammatory disease is known as PID.
- Pelvic Congestion Syndrome: Pain that is restricted to the pelvic area could be brought on by the condition called pelvic congestion syndrome. It is distinguished by swollen veins that round the ovaries and uterus and resemble varicose veins in appearance. The pelvic area contains these veins.
- Osteitis Pubis: The illness pelvic congestion syndrome may cause pelvic pain. Swollen veins around the uterus and ovaries resemble varicose veins. These veins are pelvic.
- Pelvic Bone Hydatidosis: Pelvic bone hydatidosis affects the uterus, wide ligament, and adnexa. This illness is characterised by pelvic cysts. Symptoms include stomach pain, swelling, pressure, and persistent sinus development.
- Osteogenesis Imperfecta/OI: This condition, commonly referred to as brittle bone disease, is a genetic (inherited) sickness marked by easily broken bones without apparent reason.
- Pelvic inflammatory disease: The disorder known as pelvic inflammatory disease, which goes by the same name, can harm a woman's reproductive organs. The majority of cases of this illness are caused by a sexually transmitted infection. The majority of the time, symptoms including stomach and lower abdominal pain and cervical discharge are visible.
- Pelvic Fracture: An automobile accident or other high-energy event can cause a pelvic fracture. A fall from a large height can induce this form of bone fracture, which is dangerous. Fractures to the pelvis can cause considerable bleeding and other complications that require quick medical attention. The pelvis is near major blood vessels and organs.
- Fibrous Dysplasia: Fibrous dysplasia can affect the pelvis and other regions of the body. This disease occurs when fibrous tissue replaces bone. Scar tissue that doesn't form often makes bones weaker, which raises the risk of fractures. So, the bone is more likely to break. Scar tissue can alter the bone's shape, increasing its breakability.
- Symphysis Pubis Dysfunction: Symphysis pubis dysfunction occurs when the junction between your pelvic bones (pubic symphysis) moves more than usual. 'Symphysis pubis dysfunction' refers to symptoms that occur when the joint that links your left and right pelvic bones (the pubic symphysis) moves more easily than it should.
What are some common signs or symptoms of conditions affecting the symphysis pubis?
- Pain in the pelvis, specifically around the symphysis pubis joint, might indicate a variety of health issues. Sometimes it seems like it's spreading from your stomach all the way to your hips and back. Movement difficulties may indicate a problem with the pubic symphysis.
- Having less groin mobility.
- A grinding sensation while bending or twisting at the hips.
- Discomfort in the groin or the inner thigh.
- When you walk, you experience pain or clicking noise.
- Experiencing discomfort when you move your legs, kick, stand, or sit.
- Discomfort whenever you have to contort your body in order to get to anything.
- Your doctor will be able to tell you if your symptoms are related to an issue with your pubic symphysis.
Pubic Symphysis Tests
- Stool Test: A faeces sample is examined under a microscope to check for tiny blood during a stool test. In order to look for cell abnormalities that could be brought on by cancer, this is done.
- Lower Gut Endoscopy: By inserting a lit tubing into the patient's gastrointestinal tract, a professional will perform a lower endoscopy on them. This enables the specialist to check the patient's rectum and any portion or the entire colon for indications of injury or illness.
- Ultrasound Lower Abdomen: The ultrasonography is a diagnostic procedure that creates images of a patient's interior organs using high-frequency sound waves in order to spot any fractures or abnormalities. To ascertain whether or not organs are operating normally, these images may be employed.
- MRI Lower Abdomen: Strong magnetic fields, radio waves, and computers are utilised in magnetic resonance imaging, or 'MRI,' to create precise images of the pelvic region's bones and organs.
- BMD Lower Abdomen: X-rays are used as one of the diagnostic tools in the screening for bone density, a specialised type of testing meant to assess a person's bone strength.
Pubic Symphysis Treatments
- Closed Reduction Internal Fixation: In this surgical treatment, an orthopaedic surgeon fixes shattered bones without ripping the skin open and by using several equipment.
- Pauwels Osteotomy: It is a surgical treatment used to treat femoral neck blade plate nonunion or malunion that leads to internal fixation of high femoral osteotomies. it is a reliable procedure for treating femur neck fractures and is also regarded as a conservative course of action.
- Dynamic Hip Screw Insertion: In this kind of surgery, screw hip fusions are carried out in conjunction with the recurrent fixation of femur or neck fractures. Hip screws are used for intertrochanteric fractures, and it is also a rigid fixation.
- Gallows Traction: It is a preventive fixation procedure used to treat hip dysplasia, which can cause hip fractures. In this procedure, our incubator frame is used to traction the lower hip bone, which could be made of thermoplastic. This method is used to treat thigh bone fractures in young children and puberty-aged children.
- Hip Spica Cast: It is a type of orthopaedic cast used to immobilise the hipbone when there is an injury to the hip muscles or tendons or a fracture in the hip bone. It helps heal injured hip giants and promotes the growth of fractured hip bones.
- Kuntscher Nail: It's a nail that helps stabilise the femur by connecting the femoral shaft and hipbone.
How can I keep my pubic symphysis healthy?
One of the best methods to prevent injury is to move the body in ways that won't harm the pubic symphysis joint. Exercises that build the muscles that support and protects your pelvis may also be beneficial. Any of the below may be advised by your doctor:
- Performing exercises that improve the muscle groups at the base of the pelvis (pelvic floor), the middle and lower back, the hips, the buttocks, the belly, and the vaginal wall (Kegel Exercises) may help prevent incontinence.
- When walking or jogging, reduce the strain on your joints by wearing shoes that fit your feet properly and are comfortable.
- Working out on surfaces that aren't too hard or uneven can help you avoid injury to your knees, hips, and ankles from repetitive stress. If you're worried about twisting or jamming your pubic symphysis while running, stick to flat, smooth surfaces.
- Start slowly so you don't injure yourself or overwork muscles that aren't used to doing out just yet. Taking it slow and building up to a more advanced practise is the best way to protect your joints.Preventative activities and strategies for exercising without harming yourself should be discussed with your healthcare physician.
Pubic Symphysis Medicines
- NSAIds for inflammation of Pubic Symphysis: Aspirin, naproxen sodium, and ibuprofen are a few examples of popular medications in this category. Pain in the pubic symphysis can be relieved by using indomethacin and ibuprofen together with the anti-inflammatory drugs Celecoxib, Diclofenac, Meloxicam, and Ketorolac.
- Platelet-rich plasma (PRP): A number of growth factors are released when platelet-rich plasma (PRP) is injected into a joint, usually the pubic symphysis. This accelerates the recovery of injured tissue and helps to reduce inflammation. PRP, or platelet-rich plasma, contains a variety of growth factors.
- DMARDs: Disease-modifying antirheumatic medicines treat rheumatic illnesses. Rheumatoid arthritis and other autoimmune diseases often require this family of painkillers. Methotrexate, adalimumab, baricitinib, and tofacitinib are DMARDs.
- Pregabalin: This anticonvulsant can help with neuropathy and fibromyalgia. It can also be used to treat seizures with a partial onset when combined with another seizure medication.
- Corticosteroids: Patients with specific kinds of bone disease and tendinitis that may be present in the hamstring muscle and ankle muscles may be prescribed prednisolone, hydrocortisone, corticosteroids, and other cortisone-like medications.
Table of content
Find Gynaecologist near me
Ask a free question
Get FREE multiple opinions from Doctors