Pudendal Nerve (Human Anatomy): Image, Functions, Diseases and Treatments
Last Updated: Mar 18, 2023
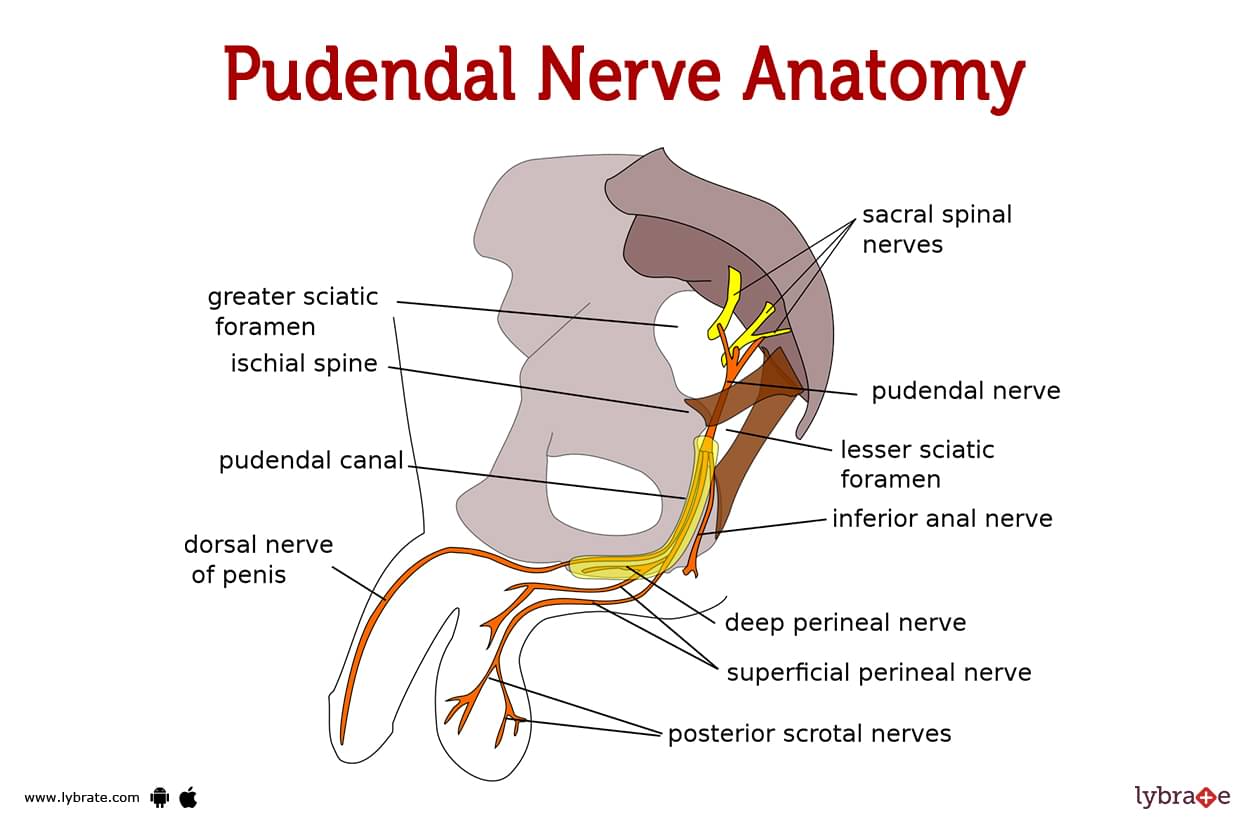
Pudendal Nerve Image
The pudendal nerve is responsible for carrying feelings from the anus and genitalia to the brain. It also controls the muscles in the sphincter that allow you to urinate and defecate.
What is the pudendal nerve?
The pudendal nerve is a nerve that delivers sensation to the vaginal region as well as specific areas of the perineum (the area between the anus and the scrotum or vulva). It is the major nerve of the perineum and carries sensory information from the genitals and anus to the brain, as well as delivering signals from the brain to the perineal muscles.
The pudendal nerve is derived from the sacral plexus, a neural network in the lower back that supplies the pelvis, lower limbs, and lower abdominal muscles. It goes via the pelvis and the pudendal canal, a small tube in the pelvis, in order to reach the genital region.
In males, the pudendal nerve transmits feeling to the scrotum, penis base, and perineum. It provides feeling to the female vulva, clitoris, and perineum. A dysfunction of the pudendal nerve can lead to numbness or altered sensation in the genital region, as well as trouble urinating and passing stool.
Where is the pudendal nerve?
One of the nerves that may be found in the pelvic area is called the pudendal nerve. It is a mixed nerve, meaning that it has both motor and sensory fibres in its make-up. It arises from the sacral plexus, which is a network of nerves located near to the lower spine in the body.
The pudendal nerve innervates the pelvic floor muscles and the skin of the perineum, which is the skin region between the anus and the genitals. Additionally, it innervates the genitalia of both males and females. This sacral plexus is an intricate neural network. These neurons provide and receive sensory and motor signals from the thighs, lower legs, foot, and a portion of the pelvis.
What is the pudendal nerve’s path?
- The pudendal nerve is a branch of the sacral plexus that originates from the S2 through S4 sacral spinal nerve roots and passes through the pelvic and gluteal (buttock) region at the upper end of the thigh bone (femur). It exits the gluteal area through the inferior sciatic foramen, a small aperture in the pelvic bone, and travels through the pudendal canal (also known as the Alcock canal), a tunnel-like hole in the pelvis.
- Alongside the pudendal artery and vein, the pudendal nerve divides into smaller branches. It is responsible for supplying sensory and motor innervation to the external genitalia, perineum, and pelvic floor muscles in both men and women.
- Dysfunction of the pudendal nerve can lead to a variety of symptoms, including pain, numbness, and weakness in the affected areas. It is always best to consult with a healthcare professional for proper diagnosis and treatment of any conditions affecting the pudendal nerve.
What are the pudendal nerve branches?
- The pudendal nerve is a special nerve in our body that helps us feel things and move certain muscles in our private areas. It has three parts called branches that each do different jobs.
- The inferior rectal nerve helps us feel and control the muscles around our bottom.
- The perineal nerve helps us feel and control the muscles in the area between our legs and around our private parts.
- The dorsal nerve of the clitoris or penis helps us feel and control the private parts that are special to girls and boys.
What is the role of pudendal nerve blocks during childbirth?
- Pudendal nerve blocks are a type of regional anaesthesia that is often used during childbirth to provide pain relief for the mother. The pudendal nerve is a branch of the sacral plexus that supplies sensory and motor innervation to the external genitalia, perineum, and pelvic floor muscles in both men and women.
- Pudendal nerve blocks are administered by injecting a local anaesthetic into the area around the pudendal nerve, which can help to numb the perineum and lower rectum and provide pain relief during childbirth.
What causes pudendal nerve problems?
There are several potential causes of pudendal nerve problems, including:
- Physical trauma: Traumatic injury to the perineum or pelvic region, such as a fall or a motor vehicle accident, can damage the pudendal nerve.
- Surgery: Surgical procedures in the perineum or pelvic region, such as prostate surgery or childbirth, can damage the pudendal nerve.
- Overuse or strain: Repetitive strain or overuse of the muscles in the perineum or pelvic region, such as during long-distance cycling or horseback riding, can lead to pudendal nerve irritation or entrapment.
- Pregnancy and childbirth: Pregnancy and childbirth can put pressure on the pudendal nerve and cause irritation or damage.
- Chronic conditions: Chronic conditions such as obesity, diabetes, or multiple sclerosis can increase the risk of nerve damage, including damage to the pudendal nerve.
Pudendal Nerve Functions
The pudendal nerve is essential for the sensation and function of the pelvic region, including the genitals and anus. This nerve is a component of the periphery of your nervous system. Peripheral nerves transmit messages from the central nervous system (brain and spine) to the extremities and specific organs.
The motor function of the pudendal nerve governs the movement of your:
- Anal sphincter muscles, which help you retain or expel faeces, are located in the anus (poop).
- Urethral sphincter muscles, which aid in the retention or release of urine (pee).
The pudendal nerve also transmits touch, pleasure, pain, and temperature information to your:
- The penis is a component of the reproductive system that is unique to men (part of the male reproductive system).
- The vaginal canal is a component of the reproductive system of women (part of the female reproductive system).
- Perineum (the skin between your anus and your vagina or penis) (the skin between your anus and your vagina or penis).
- Anus and anal canal (part of your digestive system).
Pudendal Nerve Conditions and Disorders
- Pudendal nerve damage: Pudendal nerve damage refers to damage that occurs to the pudendal nerve and can lead to sensory and motor deficits in the genital and anal regions of the body. This damage may have been brought on by an accident, an operation, or disease.
- Pudendal neuralgia: Pain in the genital or anal region is the primary symptom of pudendal neuralgia, a disorder that is most commonly brought on by irritation to the pudendal nerve or injury to the nerve itself.
- Pudendal nerve entrapment: Entrapment of the pudendal nerve is a condition that manifests itself when the nerve in question becomes compressed or entrapped, most frequently as a result of inflammation or the presence of a tumour.
- Pudendal nerve dysfunction: Pudendal nerve dysfunction is a condition that can be brought on by a number of different causes, such as a damage to the spinal cord, multiple sclerosis, or diabetes.
- Pudendal nerve irritation: Irritation of the pudendal nerve can be brought on by a number of different things, such as inflammation, infection, or the existence of a tumour. Inflammation of the pudendal nerve can cause a variety of symptoms, including numbness, tingling, or pain in the vaginal or anal region.
- Pudendal nerve stenosis: Pudendal nerve stenosis is a condition that develops when the pudendal nerve gets constricted or narrowed, most frequently as a result of inflammation or scar tissue. Pain, weakness, or trouble controlling bowel or bladder function may be symptoms of pudendal nerve stenosis. Pudendal nerve stenosis can also be caused by a pinched nerve.
- Pudendal canal syndrome: Pudendal canal syndrome is a condition that occurs when the pudendal nerve becomes entrapped or compressed within the pudendal canal, which is a small tunnel that runs through the pelvis. Pudendal canal syndrome can cause a variety of symptoms. In the vaginal or anal region, patients who have pudendal canal syndrome may experience discomfort, tingling, numbness, or weakness as symptoms of the condition.
Pudendal Nerve Tests
The diagnosis of pudendal nerve problems and the evaluation of the function of the pudendal nerve can be accomplished through the use of a variety of diagnostic procedures. These testing could include things like:
- Physical examination: During the physical examination, a healthcare provider will examine the genital and anal areas for signs of pudendal nerve dysfunction. These signs include numbness, muscle weakness, and shifts in skin colour or temperature. Additionally, the provider will examine the genital and anal areas.
- Anal manometry: Anal manometry is a test that evaluates the function of the pudendal nerve by measuring the pressure and muscular function in the anal sphincter.
- Electromyography (EMG): Electromyography, often known as EMG, is a test that monitors the electrical activity of the muscles and can assist detect whether or not there is dysfunction or injury to the nerves.
- Nerve conduction studies: This examination evaluates the function of the pudendal nerve as well as the function of other nerves in the body by measuring the speed and strength of nerve impulses.
- Magnetic resonance imaging (MRI): Magnetic resonance imaging (MRI) is a diagnostic procedure that generates high-resolution pictures of the body's internal tissues, including the pudendal nerve, by combining a strong magnetic field with radio waves.
Pudendal Nerve Treatments
There are several treatment options available for individuals with pudendal nerve disorders, including:
- Pudendal nerve decompression surgery: Pudendal nerve decompression surgery is a surgical treatment that is performed to improve the function of the pudendal nerve by relieving any pressure that may be pressing on the nerve.
- Anal sphincter repair surgery: Surgical procedure to repair damage to the anal sphincter, which is controlled by the pudendal nerve. This surgical procedure is used to repair damage to the anal sphincter.
- Physical therapy: Physical therapy is a treatment option that can be utilised to improve function and build muscle strength in the genital and anal regions.
- Nerve blocks: Injections of a local anaesthetic close to the pudendal nerve are what are known as nerve blocks. Nerve blocks are used to block pain signals. Either as a diagnostic tool to assist in determining whether or not the pudendal nerve is the cause of the pain, or as a therapeutic to provide momentary relief from the pain, this can be utilised in either capacity.
- Pudendal nerve decompression surgery: Pudendal nerve decompression surgery is a surgical treatment that is performed to improve the function of the pudendal nerve by relieving any pressure that may be pressing on the nerve.
- Anal sphincter repair surgery: Surgical procedure to repair damage to the anal sphincter, which is controlled by the pudendal nerve. This surgical procedure is used to repair damage to the anal sphincter.
- Neuromodulation: Neuromodulation is a treatment that involves modifying the activity of the pudendal nerve through the use of electrical stimulation. This treatment is used to manage pain.
How can I protect my pudendal nerves?
There are several steps you can take to protect your pudendal nerves:
- Avoid injury: Take care to avoid traumatic injuries to the perineum or pelvic region, such as falls or motor vehicle accidents.
- Use proper technique: Use proper technique when participating in activities that may put strain on the muscles in the perineum or pelvic region, such as cycling or horseback riding.
- Practise good posture: Maintain good posture and avoid sitting for long periods of time in positions that may put pressure on the pudendal nerve.
- Use caution during childbirth: If you are pregnant or planning to become pregnant, discuss pain management options with your healthcare provider to minimise the risk of pudendal nerve damage during childbirth.
When should I talk to a doctor?
You should talk to a doctor about pudendal nerve problems if you are experiencing any of the following symptoms:
- Pain in the perineum, anus, or genital area
- Numbness or tingling in the perineum, anus, or genital area
- Weakness in the muscles of the perineum or pelvic floor
- Difficulty urinating or defecating
- Sexual dysfunction or decreased sensation in the genital area
- These symptoms may be caused by a variety of factors, including pudendal nerve problems. It is important to consult with a healthcare professional for proper diagnosis and treatment.
Pudendal Nerve Medicines
- Analgesics for pain in the pudendal nerve: Analgesics, often known as pain drugs, are sometimes prescribed to patients suffering from pudendal nerve problems in order to alleviate their discomfort. Analgesics like acetaminophen, tramadol, and opioids like codeine and oxycodone are a few examples of the kind of medications that could be utilised.
- Muscle relaxant for stiffness of pudendal nerve: Individuals who suffer from pudendal nerve diseases may benefit from the usage of muscle relaxants in order to alleviate stiffness and enhance muscle function. Cyclobenzaprine, carisoprodol, and diazepam are some examples of muscle relaxants that might be utilised in this situation..
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen and naproxen are two examples of drugs that could be taken to alleviate pain and inflammation.
- Antidepressants for pudendal nerve: Medications such as selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants may be prescribed to patients in order to alleviate the symptoms of chronic pain.
- Anticonvulsants for pain of pudendal nerve: Medications like gabapentin and pregabalin, among others, are a potential treatment option for managing chronic pain.
- Antibiotics for infection of pudendal nerve: Illnesses that affect the pudendal nerve can be treated with these drugs. Some examples of such infections are an infection of the urinary system or an infection that is transmitted sexually.
Table of content
Find Neurologist near me
Ask a free question
Get FREE multiple opinions from Doctors