Rectal prolapse: Causes, Symptoms, Treatment and Cost
Last Updated: Mar 09, 2023
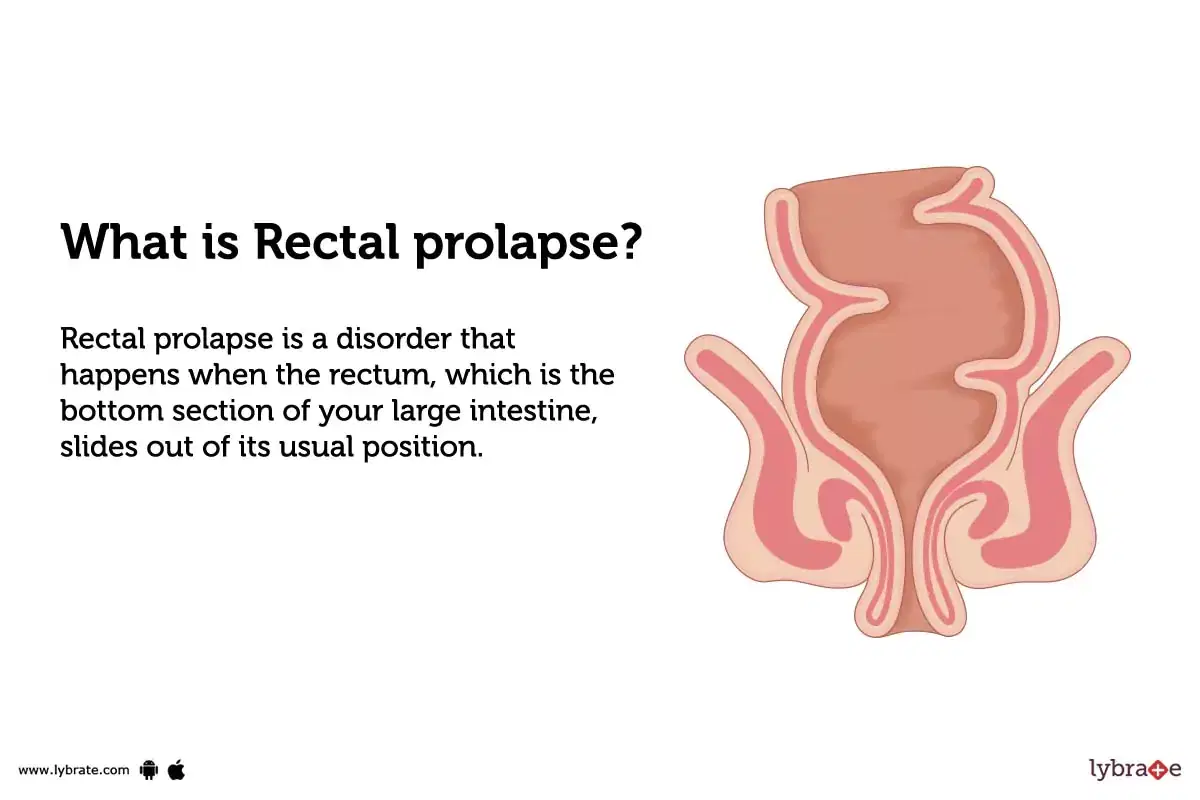
What is Rectal prolapse?
Rectal prolapse is a disorder that happens when the rectum, which is the bottom section of your large intestine, slides out of its usual position. This allows the walls of the rectum to protrude through the anus, which is the opening at the top of your large intestine. It is most common in women between the ages of 45 and 54, but it can affect men as well.
Types of Rectal prolapse
There are three types of rectal prolapse:-
- Complete Rectal Prolapse: This is a disorder where the entire wall of the rectum passes through the anal opening. The rectal wall can be seen externally; it may cause difficulty with bowel movements and leakage of mucus or faeces from the anus.
- Partial Rectal Prolapse: This involves only part of the wall pushing through to the outside and is most commonly seen in children with tissue around the inside edge of anus stretched out thin enough to allow part protrusion (intussusception).
- Mucosal Rectal Prolapse: This occurs when only a portion or mucosa layer slips outwards. Mucosal prolapse are more common among children due to their weakened pelvic muscles from recent childbirth, constipation or straining during a bowel movement; It often resolves on its own without any intervention.
What causes Rectal prolapse?
- Rectal prolapse is caused by weakening of the connective tissues and muscles in the rectum.
- It can be caused by chronic constipation, straining during childbirth or severe coughing, muscular dystrophy or neurological disorders that make it difficult to control anal muscles.
- It can also result from changes in normal tissue due to old age, long-term diarrhoea or obesity.
What are the symptoms of Rectal prolapse?
- Rectal prolapse can cause feelings of pressure in the rectum, a lump at the anus, leakage of mucus or stool, or difficulty controlling bowel movements.
- Physical signs include an enlarged single protrusion from the rectum when bearing down or standing, visible reddening of the skin around the anus and difficulty inserting a finger between the mass and anal sphincter.
- Other associated symptoms may include faecal incontinence (inability to control gas or bowel movement), constipation and pain in lower abdomen.
How can you prevent Rectal prolapse?
- Engage in regular physical activity to keep core muscles strong.
- Add high fibre foods to the diet to avoid straining during defecation.
- During bowel motions, you should try to avoid straining or holding your breath.
- Stay away from intense activities like heavy lifting and anything that places a strain on your stomach.
- Maintain a healthy weight to reduce abdominal pressure.
- Consume a lot of water and other fluids during the course of the day.
- Change positions often, especially when sitting for long periods of time.
Rectal prolapse - Diagnosis and Tests
- Physical Examination:A physical exam will be done to inspect the protrusion of the rectum outside of the anal opening.
- Imaging Tests:Imaging tests like X-rays and MRIs can help diagnose rectal prolapse and assess any associated damage or deformity that may have occurred.
- Anoscopy:Anoscopy is a procedure that helps to examine the anus, lower rectum, and pelvic floor muscles. During the procedure, a doctor will insert a short, thin tube (called an anoscope) into the anus to examine its lining and assess any abnormal growths or problems.
- Proctosigmoidoscopy:Proctosigmoidoscopy is a medical procedure wherein a doctor inserts a thin, lighted tube with a camera (called an endoscope) into the anus and rectum. Rectal prolapse is a condition in which the rectum and sigmoid colon, both of which are engaged in the digestive process, may be seen by the doctor via the tube.
- Colonoscopy:Colonoscopy may be used to diagnose and evaluate rectal prolapse.During the operation, a thin, flexible tube that is attached to a light and camera is threaded through the anus. This allows the doctor to view the rectum and colon, while also helping them to identify any visible signs of prolapse.
What are possible complications of Rectal prolapse?
- During bowel motions, one experiences pain as well as blood.
- Damage to the anus and rectal wall.
- Difficulty controlling bowel movements or passing stool.
- Incontinence of faeces or soiling of the underpants may occur.
- Infections, including urinary tract infections (UTIs) and yeast infections
- Anal leakage when passing gas.
- Formation of tear in the muscles surrounding anus.
- Obstruction of the intestines.
Home Remedies for Rectal prolapse
- Drink Saunf (Fennel) Decoction: A decoction may be made by bringing one teaspoon of fennel seeds and one cup of water to a boil. Let it cool and drink it daily to relieve symptoms of rectal prolapse.
- Add Garlic: Add one teaspoon garlic powder to a cup of fresh milk and drink it twice daily for at least one month.
- Eat Amalaki Fruits: Eat 5-6 amla fruits daily and follow this routine for 3-4 months for better results.
- Take Raisins: Boil 3 tablespoons of raisins in a litre of water till half the amount is left, strain the liquid, let it cool and have it 2-3 times in a day after meals for healing rectal prolapse naturally.
- Ashwagandha: The Ayurvedic herb, Ashwagandha can be made into tea and drank 2-3 times per day to reduce symptoms of rectal prolapse.
What to eat in Rectal prolapse?
- Eating a healthy diet is important for maintaining general health and strength, as well as helping to manage the symptoms of rectal prolapse.
- A person should aim to consume foods rich in fibre and liquid, such as fruits, vegetables, nuts, beans, pulses and whole grains. This can help reduce constipation, which is a common risk factor for rectum prolapse.
- Eating plenty of probiotic-rich foods could also help improve digestion and reduce the impact of some symptoms associated with rectal prolapse such as urinary frequency and urgency while improving overall digestive health long term.
What not to eat in Rectal prolapse?
In rectal prolapse, it is important to avoid a diet high in fat and processed foods, as well as foods that may be difficult to digest such as spicy, gas-producing, and highly acidic items. Examples of such foods include:
- Fried or fatty meats (such as burgers or bacon).
- Excess sugar and sugary products.
- Highly salty processed snacks.
- White breads, pastas, and other refined carbohydrates.
- Caffeinated beverages.
- dairy items such as cheese and whole milk are examples of these goods.
- Beverages with carbonation and soft drinks.
Rectal prolapse Treatment
- Manual replacement:Manual replacement is a procedure to manually push the prolapsed rectum back into its normal position inside the body. The procedure is usually done with careful guidance from an experienced medical provider.
- Supportive devices:Supportive devices may be used to help reduce rectal prolapse. These devices help to hold the rectum in place, preventing it from slipping out further or recurring.
- Medications:Medications alone are not often effective in treating rectal prolapse, but can be used in combination with lifestyle changes, such as increasing fibre intake or avoiding straining during bowel movements. Common medications used to treat this condition include laxatives and stool softeners to help soften the stool, reduce straining and provide relief from constipation.
- Pectopexy:Surgically reattaching the prolapsed rectum by fixing it to the tailbone (sacrocolpopexy).
- Sacral Rectopexy:Anchors the rectum to the sacrum with sutures, meshes or anchors made of synthetic materials.
- Staged repair:Sutures and stitches are used to attach the prolapsed rectum to muscle and connective tissue in multiple steps.
- Abdominoperineal or laparoscopic resection:Removes a portion of the large intestine and reattaches it in its correct anatomical position between two healthy parts of the intestine creating a new end where stool can exit the body, requiring patient to have external bag for faeces collection.
Which doctor to consult for Rectal prolapse?
It is important to seek medical advice from a doctor specialising in disorders of the intestines and rectum (proctologist) as soon as possible to determine treatment options for rectal prolapse.
Which are the best medicines for Rectal prolapse?
- Alpha-agonists:These drugs work by relaxing the muscles of the rectum, allowing it to slip back in place. Examples include oxybutynin and phenoxybenzamine.
- Laxatives:These are medications that can help prevent constipation and make bowel movements easier. Examples include lactulose, polyethylene glycol, and docusate sodium.
- Topical steroids:These drugs reduce inflammation that might be contributing to rectal prolapse by inhibiting the immune response around the rectum. Examples include hydrocortisone and prednisolone acetate.
- Estrogens:Estrogens are hormones that can help bolster the strength of abdominal muscles around the rectum, allowing it to stay in place better than before taking the medication. Examples include conjugated estrogens, ethinyl estradiol, and estradiol cypionate injection.
- Antispasmodics:These drugs relax smooth muscle spasms in gastrointestinal tissues and may ease irritation or inflammation associated with a rectal prolapse event.
How long does it take to recover from Rectal prolapse?
Recovery from rectal prolapse typically takes several weeks to months depending on the severity of the prolapse and if any additional treatment is needed. It is essential that patients maintain close contact with a doctor to ensure successful recovery.
Are the results of the treatment permanent?
The severity of the illness and the kind of prolapse both have a significant role in determining how effective therapy can be.
Generally, surgery is the most effective treatment for this condition and may result in a permanent resolution. However, further problems can develop if there is an underlying cause for the prolapse such as an ongoing chronic condition or trauma during childbirth or advanced age that has weakened the anal sphincter muscle.
Alterations to one's way of life are sometimes suggested as a means of alleviating symptoms and maybe warding off the need for surgical treatment.
What are post-treatment guidelines?
- Rest and minimise physical activity immediately following surgery.
- Take medications as prescribed, such as pain relievers and antibiotics (if needed).
- Applying ice to the region will help lessen the swelling and the pain.
- After surgery, you should wait between four and six weeks before straining or carrying heavy objects.
- Wear a protective support device (e.g., a brace) for several weeks after surgery, if indicated.
- Perform pelvic floor muscle contraction exercises regularly to strengthen the muscles of your pelvic floor and help prevent recurrence of rectal prolapse symptoms if recommended by your doctor/healthcare provider.
- Monitor your bowel movements at home and report any changes or significant blood loss in stools to your healthcare provider.
- Follow up with your doctor for routine checkups in order to monitor recovery.
What is the cost of Rectal prolapse treatments in India?
It is possible for the price of therapy for rectal prolapse in India to change based on the severity of the problem as well as the treatment option that is being sought.
Generally, non-surgical treatments such as medication, lifestyle changes and pelvic floor exercises are considered first and are typically low-cost options. For more severe cases, surgery may be recommended, which can cost anywhere from Rs 1 Lakh to Rs 5 Lakh or more depending on the type of operation.
What are side-effects of Rectal prolapse treatments?
- Postoperative pain:Mild to moderate postoperative pain is common after rectal prolapse treatments, and can usually be managed with low dose pain medications.
- Bleeding:Bleeding from the site of surgery is also a common side effect, but usually resolves within two to three days.
- Abdominal cramping:Some patients may experience abdominal cramping during and after treatment, which can be managed with medications and lifestyle modifications.
- Bowel dysfunction:Treatment for rectal prolapse may cause temporary changes in bowel habits, such as constipation, diarrhoea or both.
- Risk of infection:As with any surgery, there is a risk of infection at the site of treatment which may require antibiotics and further treatment to resolve properly.
Rectal prolapse - Outlook/ Prognosis
In order to avoid issues like 'Damage to the anus and rectal wall, blockage of the intestine,' which can take months or years to repair depending on how severe the problem is, you should visit a doctor in your area if you are experiencing any rectal prolapse-related difficulties.
Table of content
15+ Years of Surgical Experience
All Insurances Accepted
EMI Facility Available at 0% Rate
Find General Surgeon near me
Ask a free question
Get FREE multiple opinions from Doctors