Testis (Male Anatomy): Image, Function, Diseases, and Treatments
Last Updated: Mar 14, 2023
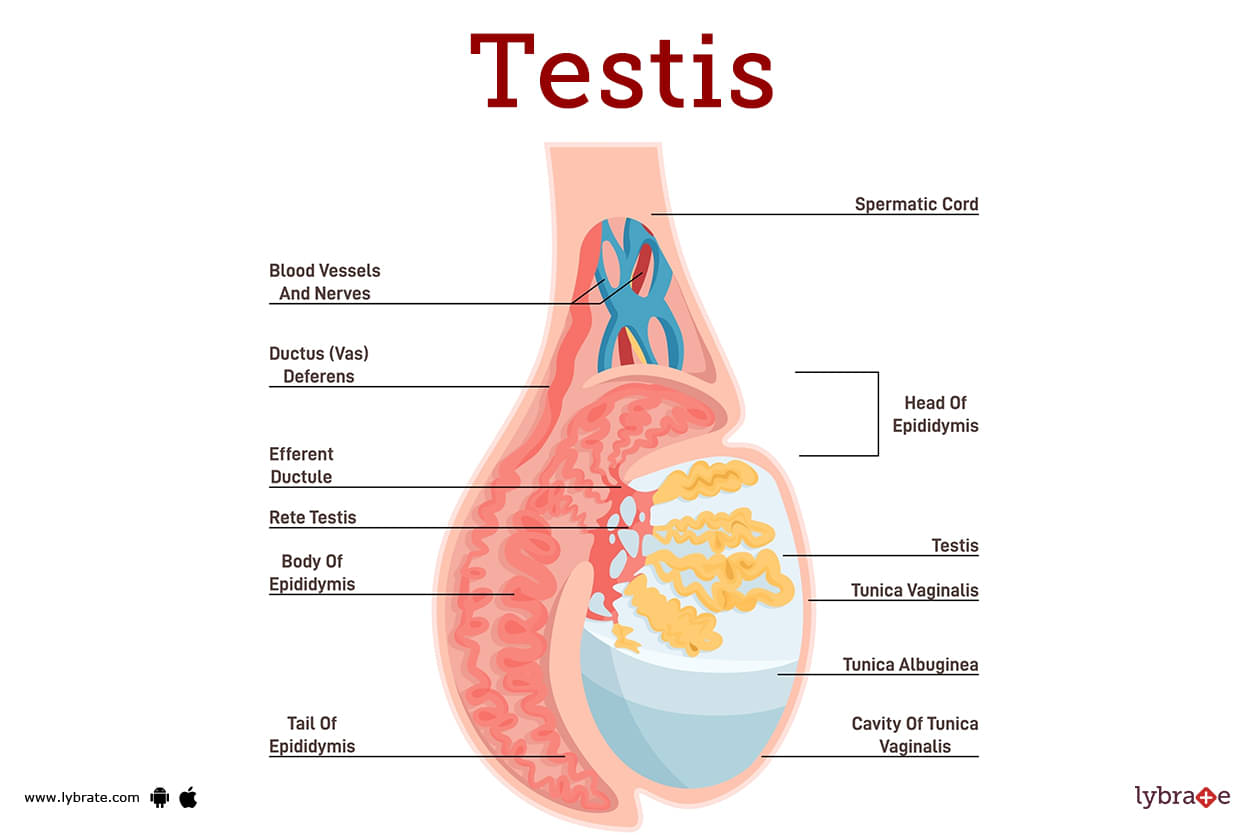
Testis Image
The testis is a male gonad. It is homologous to the female ovary. It is a mobile organ found in the scrotal sac's two halves. The testis generates spermatozoa and secretes testosterone (or dihydrotestosterone), a male hormone that is responsible for the development and maintenance of secondary sex characteristics in males.
It is compressed from side to side and has an oval/ellipsoid shape.The average testicular dimensions are 5 cm long, 2.5 cm wide, and 3 cm tall (anteroposterior diameter). The testis is suspended in the scrotum by the spermatic cord. The upper pole is slightly forward and laterally tilted, while the lower pole is slightly backward and medially tilted.
Function of Testis
The primary functions of the testes are, respectively, the creation of sperm and the preservation of sperm. In addition, they are necessary for the generation of testosterone in addition to many other androgens, which are male hormones.
The unique ovular shape of the testes can be attributed to the lobules, which are the tissues that make up the testes. Strong connective tissue wraps itself around the entire structure, encasing the coiled tubes that make up lobules and protecting them from the environment.
Diseases of Testis
- Hydrocele: Hydrocele is characterised by fluid collection within the tunica vaginalis. While testicular irritation can lead to hydrocele formation because of the tunica vaginalis' proximity to the organ, idiopathic causes account for the vast majority of hydroceles. Inserting a small trocar and later a cannula through the skin of the scrotal region allows for the drainage of fluid from the tunica vaginalis.
- Varicocele: To put it simply, varicocele is a medical disorder in which the veins of the pampiniform plexus grow enlarged, convoluted, and elongated. A varicocele is the medical term for this issue. Most people in this age range (teens and young adults) suffer from this disorder. We can explain why the left side has a much greater incidence rate by considering the following.
- Tumours of the testis: Seminoma, also known as carcinoma of the seminiferous tubules, is the most common type of testicular tumour, and teratoma is the second most common type of testicular tumour. The more prevalent of the two forms is seminoma (malignant change in the totipotent cells). Secondary tumours in the abdomen developed after cancer cells spread from the testis to the lumbar (pre- and para-aortic) lymph nodes at the level of the L1 and L2 vertebrae via the lymphatic system.
- Torsion of the testis: In medical terms, a torsion of the testis is when the spermatic cord is twisted within the scrotum. The result is a twisted testis. Extreme pain is the hallmark of this condition, which strikes young adults and physically active youngsters frequently.
- Cryptorchidism (incomplete descent of testis): Incomplete testicular descent, or cryptorchidism, is a condition that manifests itself when the testis fails to descend all the way to the scrotal base during normal development.
- Ectopic testis (maldescent of the testis): Maldescent of the testis, or ectopic testis, is a condition in which one or both testes fail to reach the scrotum after being routinely transported to that region of the body. So, it might be in any of the four possible spots:
- Scrotal edema: Due to the pliability of the skin and the dependent position of the scrotum, edema commonly develops there.
- Sebaceous cysts: Because of the high concentration of hair and sebaceous glands in the scrotum, this area of skin usually develops many sebaceous cysts. Because of this, sebaceous cysts are frequently found on scrotal skin.
- Scrotal elephantiasis: Massive growth and swelling of the scrotum characterise the medical disorder known as scrotal elephantiasis. Because the slender worms associated with filariasis obstruct lymph vessels, the interstitial fluid that normally circulates in the scrotal wall accumulates there, leading to the dramatic swelling and enlargement shown here (Wuchereria bancrofti).
- Orchitis: If your testicles are swollen or inflamed, you may have orchitis, a medical condition. Like its close cousin epididymitis, orchitis is most often the result of a STI-caused illness (STD). Symptoms of orchitis include a decrease in sperm count, testicular pain, swelling, fever, nausea, and vomiting.
- Hypogonadism: When your body does not create enough testosterone, a condition known as hypogonadism sets in. There could be an issue with your testicles, or maybe your brain isn't properly triggering the production of hormones.
- Testicular cancer: Thousands of American men over the age of 18 are diagnosed with testicular cancer every year. The survival rate for testicular cancer is rather low, and the disease has a high cure rate. This tumour is unusual in that it typically affects young men. A non-painful tumour on one of the testicles is a symptom of testicular cancer. Back pain, a heavy sensation in the scrotum, a dull ache in the groyne, and a generalised lack of energy are all common symptoms.
- Spermatocele: An abnormal sac (cyst) called a spermatocele (SPUR-muh-toe-seel) can form in the epididymis, a small, coiled tube on the top of the testicle responsible for collecting and transporting sperm. An abnormal sac called a spermatocele (SPUR-muh-toe-seel) forms in the epididymis. There is no need for worry, as spermatoceles are painless and cancerous growths they do not spread. Milky or transparent fluid, which may contain sperm, fills it normally.
- Contralateral testicular cancer: A metachronous contralateral testicular tumour is more likely to develop in patients who have had a testicular germ cell tumour (TGCT) diagnosed (CLTT). As much as 15 times more likely to develop a CLTT than the general population, TGCT patients are at a much higher risk for this complication. While the risk is two times as great after a seminoma as it would be after NSGCT, it steadily decreases with each cycle of chemotherapy. It is advised that high-risk individuals constantly assess their own health.
- Fournier's gangrene: Fournier's gangrene is a bacterial infection of the perineum, scrotum, or penis (the region between your genitalia and rectum) that can be deadly if left untreated.). This infection spreads rapidly and needs medical intervention right away.
- Testicular feminization syndrome: A syndrome characterised by the progressive feminization of the testicles. In a genetic guy (someone with one X chromosome and one Y chromosome), androgen insensitivity syndrome (AIS) can be defined as a resistance to the effects of male-associated hormones like testosterone.). This individual thus has some feminine physical traits yet a masculine genetic make-up.
- Klinefelter's syndrome: When a male child is born with an extra X chromosome, the result is known as Klinefelter syndrome.
- A typical male has two chromosomes: one X and one Y. Klinefelter syndrome can cause a variety of symptoms, including enlarged breasts, breast cancer, osteoporosis, infertility, and intellectual disability. Hormone replacement, talk therapy (both physical and mental), and physical therapy are frequently used to treat this illness.
- Intratubular germ cell neoplasm (ITGCN): It is intratubular germ cell neoplasia that serves as the precursor lesion for invasive testicular germ cell tumours (TGCTs) in adolescents and young adults (ITGCN). This surge in tumours has prompted much research on ITGCN's origins, diagnostic tools, and therapeutic avenues.
Test for Testis
- Physical Exam: Analyze the Patient's Physical State Finding lumps, swelling, or other abnormalities on or in the area of the testes might be aided by a thorough examination of the patient's physical condition. In this case, palpation may be necessary (the light touching of tissues). Your doctor may also examine your testicles for pain or abnormal movement by having you move your leg, pelvis, or torso. Testicular torsion detection may necessitate this procedure.
- Ultrasound: Testing the testicles with an ultrasound is the most common procedure. The scrotum is scanned with sound waves to check for abnormalities in a noninvasive examination. Testicular torsion, testicular cancer, and varicocele can also be ruled out or detected, as can abnormal blood flow.
- Magnetic resonance imaging: Using strong magnetic fields and radio waves, magnetic resonance imaging (MRI) creates incredibly clear pictures of organs and tissues. The diagnostic procedure of choice for cryptorchidism is magnetic resonance imaging (MRI). In addition, it can help doctors identify cancerous tumours from less dangerous benign ones.
- C.T. (Computed Tomography): Computed tomography (CT) also known as: Using a combination of x-ray and computer technologies, a computed tomography (CT) scan provides an in-depth look of the inside components of the body to aid in diagnosis. It's capable of taking pictures from a wide range of angles. As a result of the computer putting them all together, a 3D image is formed.
- Blood test: We're going to do some tests on your blood to look for specific proteins. These proteins, known as tumour markers, can be used in the detection of testicular cancer.
- X- ray: With the use of the examination photographs, they will be able to spot anomalies that could indicate malignancy. Cysts, turmos, and torsions are all diagnosable by these procedures.
- Testicular Biopsy: Obtaining sperm for in vitro fertilisation or determining the cause of male infertility are just a few of the many potential applications of a testicular biopsy. The exact position and health of a testicular mass can be determined with a biopsy (IVF).
- P.C.R: Polymerase Chain Reaction (or P.C.R. for short) is a technique that can be used to determine which microorganisms are responsible for damage to the male copulatory organ. Chlamydia and Gonorrhea are only two examples of the kinds of bacteria that can cause such infections. And there are many disorders that can be diagnosed using PCR.
- Microscopic examination: Microscopical inspection is one approach to diagnosing infectious conditions like bacterial inflammation.
Testis Treatment
- Radiation: By exposing patients to large doses of energy, radiation therapy kills testicular cancer cells while minimising damage to good tissue.
- Implantation of radioactive seeds: For cancers of the testicles, radioactive seeds must be implanted in the area for radiation to be delivered from the outside in.
- Chemotherapy: Chemotherapy, or chemotherapy, is a method of treating cancer that involves the administration of one or more anti-cancer drugs in accordance with a predetermined schedule. Chemotherapy can be given for many different reasons, including curing the disease, extending life, and relieving symptoms.
- Hormone treatment: As a component of hormonal therapy, human chorionic gonadotropin, also known as hCG, is a peptide hormone that can be administered either subcutaneously or intramuscularly (HCG). If your son takes this hormone, there is a chance that his testicle will transfer from his testicle to his scrotum. Because the success rate of hormone therapy is so much lower compared to that of surgical procedures, one should only consider using it as a last resort.
- Orchiopexy: The orchiopexy surgical approach, which is the most common surgery for treating a single descending testicle, has a success rate that is very near to one hundred percent. While fertility rates are somewhat typical for men who have surgery with one undescended testicle, they drop to 65% for those who have two. Having surgery can reduce your risk of developing testicular cancer, but it won't remove it totally.
Medicine for Testicular Disorder
- 5-alpha-reductase inhibitors: Medication known as a 5-alpha-reductase inhibitor is prescribed for men. These medicines are able to perform their function by inhibiting 5-alpha-reductase, as their name implies. One way they do this is by reducing the amount of a specific type of testosterone in the body. Reduced levels of DHT in the body lead to a smaller prostate and better urine flow. It's because DHT is made in the prostate.
- Flutamide for cancer: Testicular cancer is routinely treated with this androgen receptor and antagonist. However, gynecomastia, breast soreness, and erectile dysfunction are some of the negative consequences that can occur. Cancer patients can benefit from using flutamide.
- Ciprofloxacin: The fluoroquinolone ciprofloxacin is the gold standard for treating chronic inflammation in the area of the testes. The medication's brand name is Ciprofloxacin.
- Amoxicillin for bacterial infection: Drugs like amoxicillin, which are used to treat bacterial infections, need to be kept in a sterile environment to prevent the spread of bacteria to healthy cells during storage.
- Cisplatin: In the treatment of testicular cancer, cisplatin has become one of the most widely recognised use of the drug as a chemotherapeutic agent. Few alternatives existed for treating men with testicular cancer before the development of cisplatin. Ovarian, lung, bladder, and cervical cancers are just a few of the many for which cisplatin is used in treatment.
Frequently Asked Questions (FAQs)
What are 5 warning signs of testicular cancer?
What is the most common testicle problem?
What causes testicular disease?
What happens when testis are damaged?
Can testicle problems be cured?
What can cause testicle problems?
Which disease is caused by testes?
How do you cure testicular problems?
Can testicle problems be cured at home?
Table of content
Find Sexologist near me
Ask a free question
Get FREE multiple opinions from Doctors